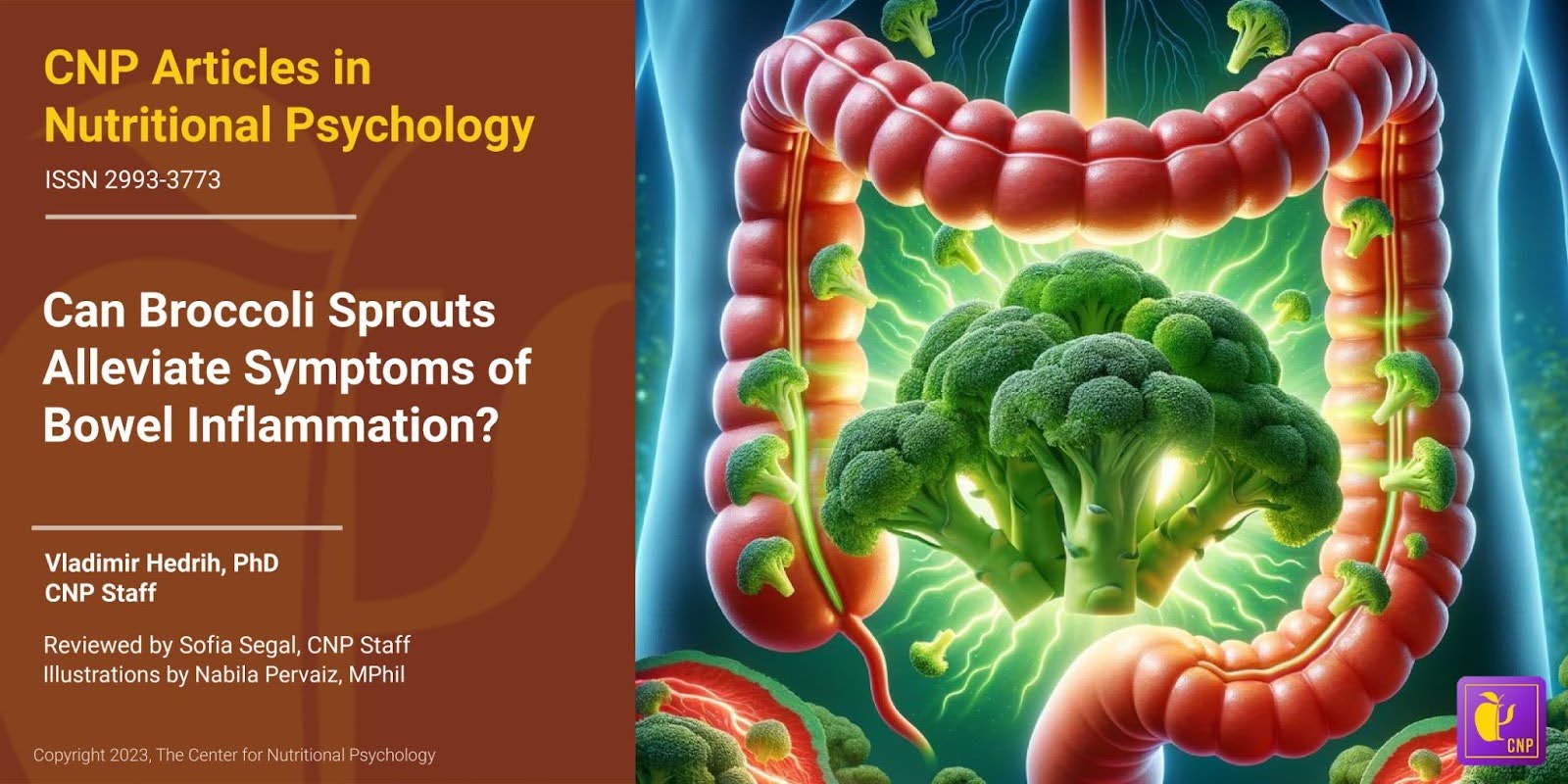
- A study published in mSystems found that feeding mice a diet consisting of 10% steamed broccoli sprouts alleviated the symptoms of experimentally induced bowel inflammation
- These mice gained more weight during the study period
- The mice showed lower inflammation indicators and richer bacterial communities in all parts of the gut compared to mice with induced bowel inflammation but on a regular diet
Inflammatory bowel diseases
Inflammatory bowel diseases constitute a group of chronic, inflammatory disorders primarily affecting the gastrointestinal tract. The two main types of these diseases are Crohn’s and ulcerative colitis. Both conditions arise from an abnormal immune response in which the immune system mistakenly attacks healthy cells lining the digestive tract, leading to chronic inflammation (see Figure 1).
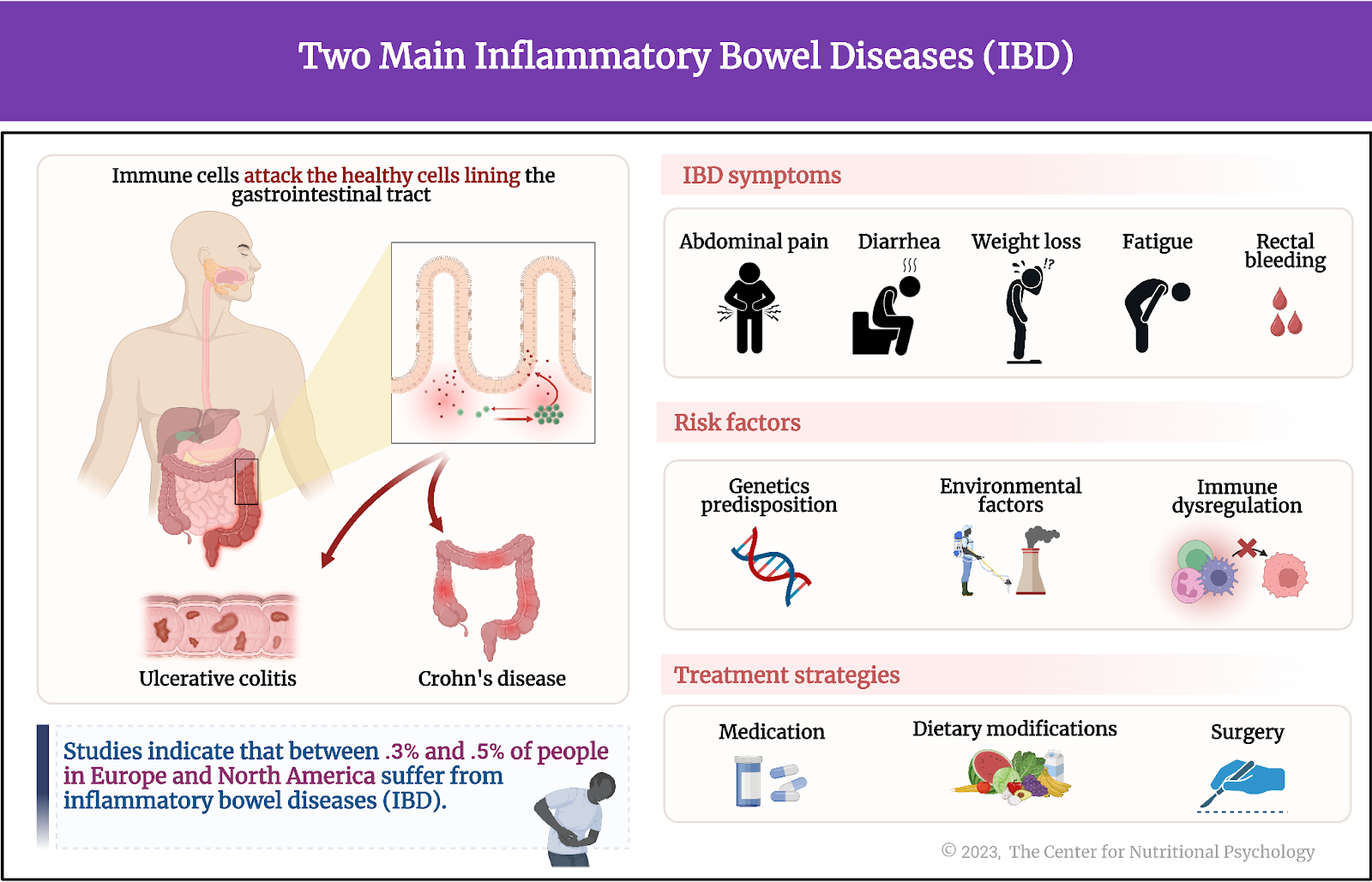
Figure 1. Two main inflammatory bowel diseases
Symptoms of inflammatory bowel diseases can include abdominal pain, diarrhea, weight loss, fatigue, and sometimes rectal bleeding. These diseases are complex conditions usually caused by multiple factors. Genetic predisposition, environmental factors, and immune system dysregulation play a role in their development (Ramos & Papadakis, 2019). While there is currently no cure for inflammatory bowel diseases, various treatments such as medications, dietary modifications, and, in some cases, surgery can help manage symptoms and improve the quality of life for individuals suffering from them (Holman et al., 2023).
Could inflammatory bowel disease symptoms be improved through diet?
Studies indicate that between 0.3% and 0.5% of people in Europe and North America suffer from inflammatory bowel diseases (Ng et al., 2017). While these percentages might seem small, they represent millions of individuals worldwide. Considering that these diseases’ symptoms are often devastating, it is quite understandable that finding ways to treat inflammatory bowel diseases has attracted much research attention.
A significant portion of this research focused on identifying dietary elements that could alleviate the symptoms of these diseases because changing a diet is considered an easy way to address symptoms if a viable dietary approach existed. In this regard, cruciferous vegetables are seen as a promising avenue of research, as their consumption is associated with reduced inflammation and a lower risk of cancer (Holman et al., 2023; Tilg, 2015). Some common cruciferous vegetables include broccoli, cauliflower, cabbage, Brussels sprouts, kale, and collard greens.

Broccoli sprouts
Broccoli sprouts are young, edible shoots that grow from germinated broccoli seeds. They are known for their high nutritional value, particularly for being rich in glucosinolates –compounds that can be converted into bioactive substances with potential health benefits, including antioxidant and anti-inflammatory properties. The presence of glucosinolates is particularly high in immature broccoli sprouts.
One of these bioactive substances is sulforaphane. Studies have shown that sulforaphane inhibits the action of certain immune factors responsible for the upregulation of proinflammatory proteins in the body, known as cytokines.
However, when broccoli is eaten raw, enzymes in it will convert most glucosinolates into an inactive substance. Steaming or cooking fresh broccoli sprouts alters these plant enzymes’ activity and leaves glucosinolates intact. This allows a specific type of gut bacteria to convert glucosinolates into sulforaphane (Holman et al., 2023) (see Figure 2).
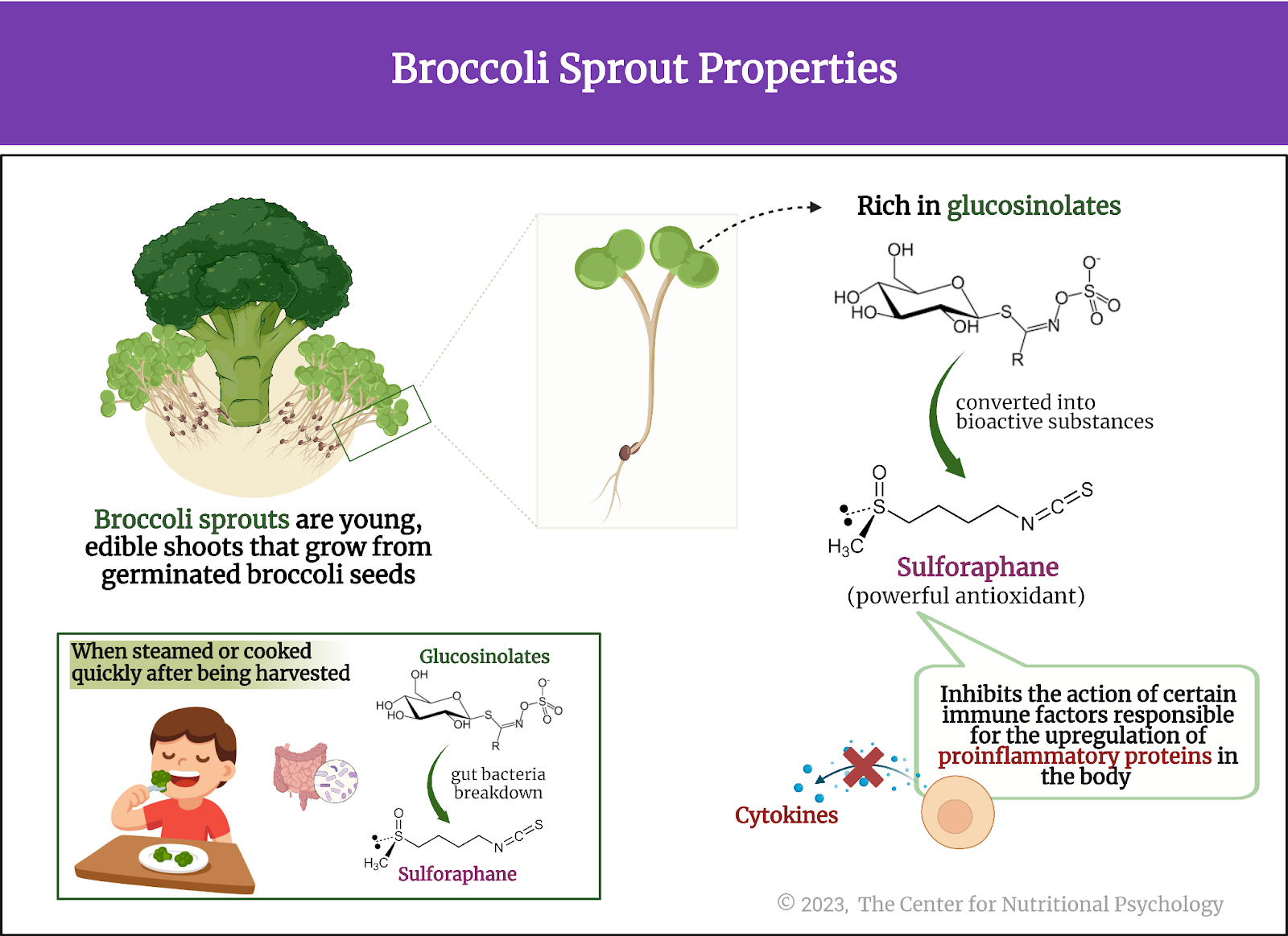
Figure 2. Broccoli sprout properties
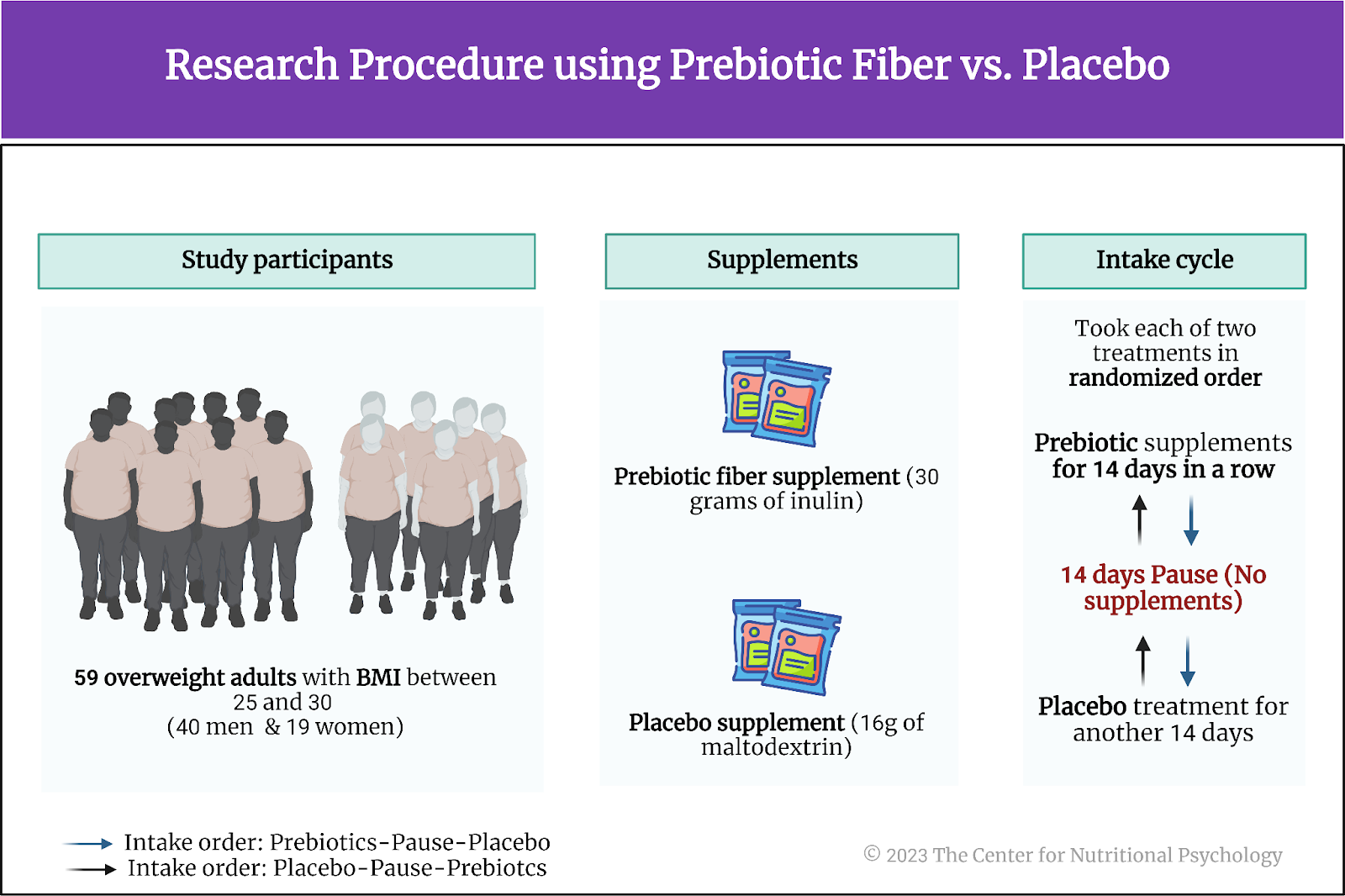
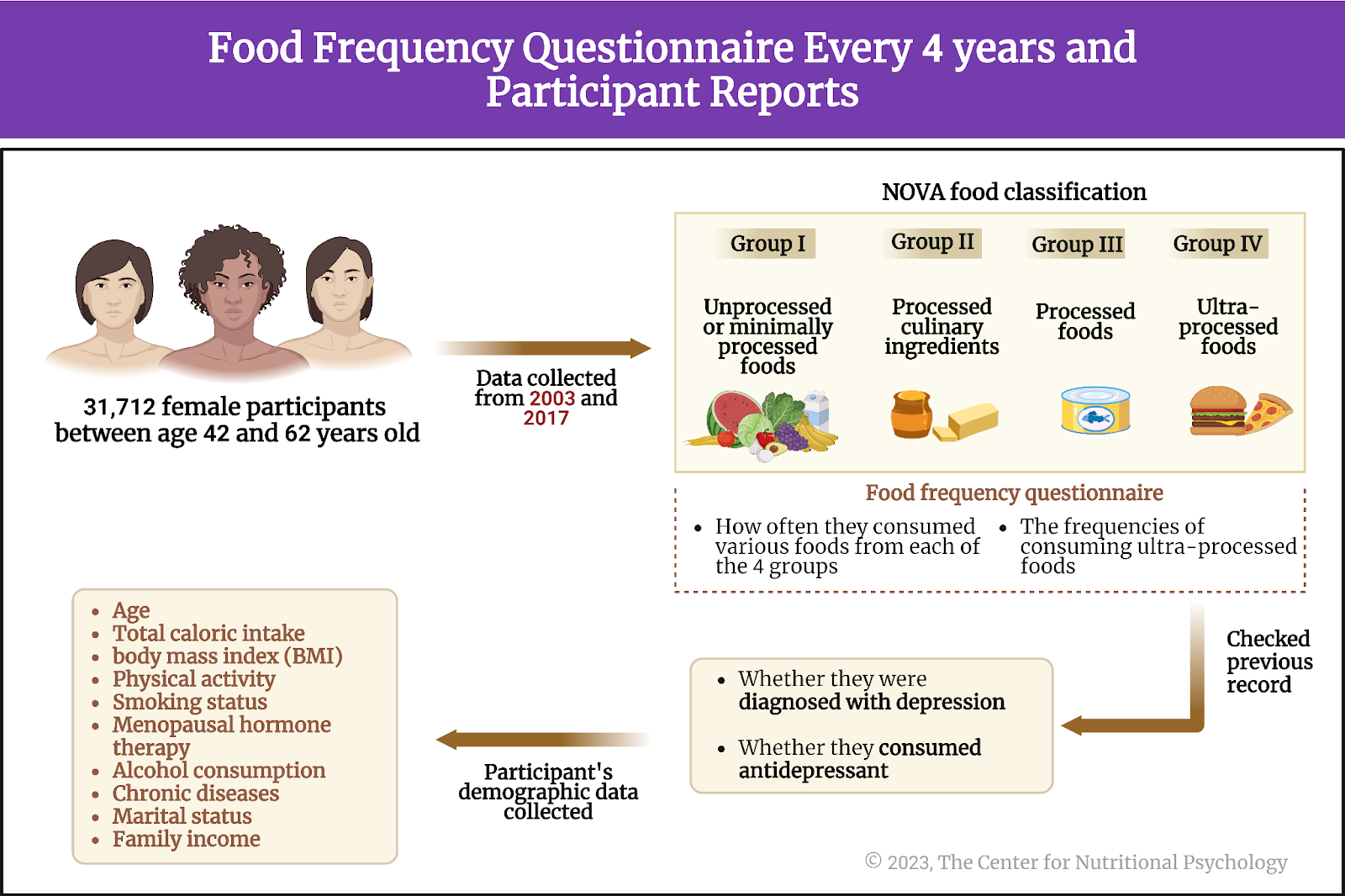
The current study
Study author Johanna M. Holman and her colleagues aimed to investigate whether adding steamed broccoli sprouts to mice’s diets could improve chronic, relapsing colitis symptoms. Simultaneously, they wanted to see how these sprouts affect gut microbiota composition under the same conditions.
Gut microbiota, also known as gut flora or gut microbiome, is the diverse community of microorganisms, including bacteria, viruses, fungi, and archaea, that inhabit the gastrointestinal tract of humans and other animals. They play a crucial role in digestion and metabolism, being also involved in several other bodily functions (Carbia et al., 2023; Leclercq et al., 2020).
The procedure
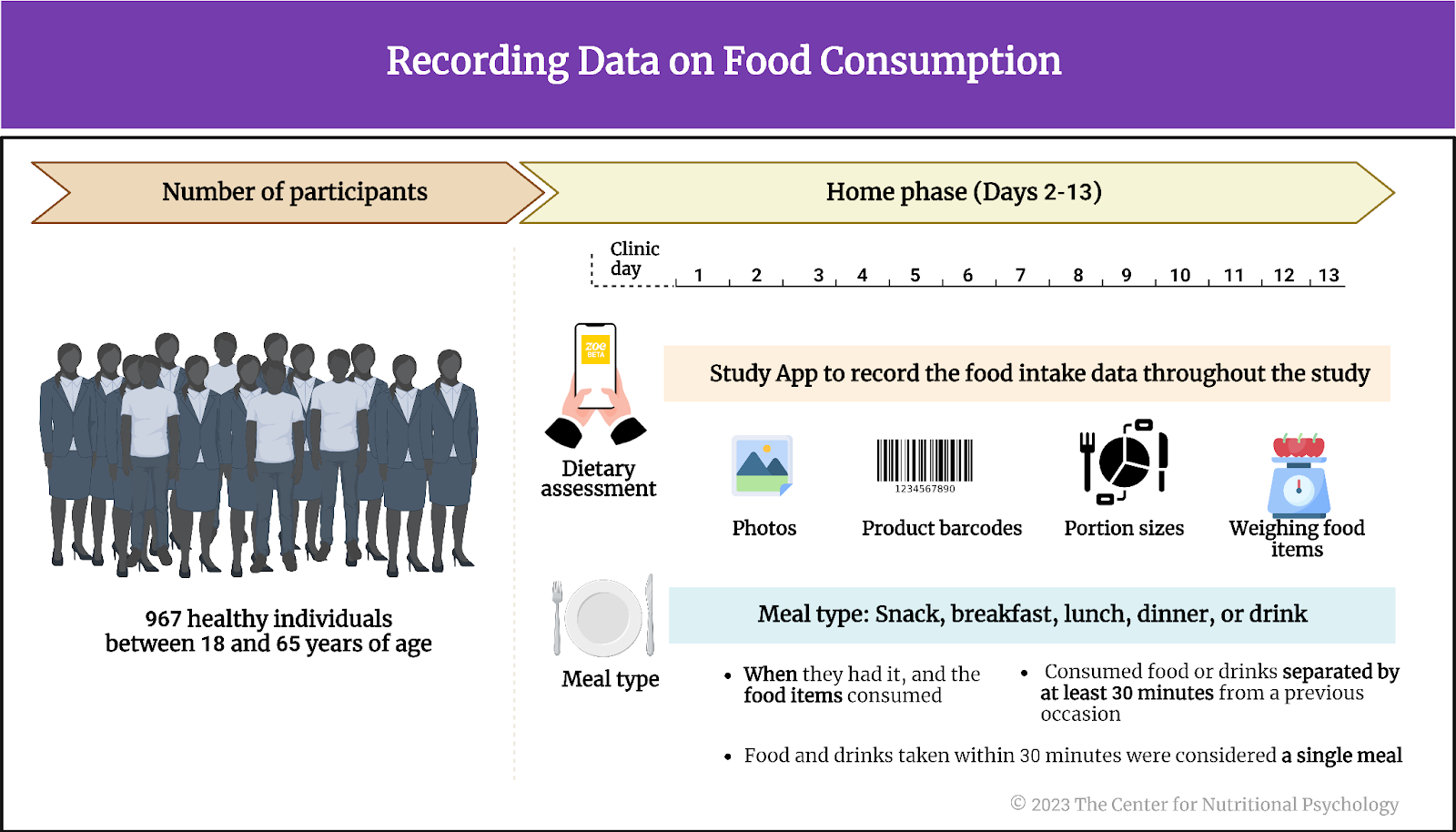
The study was conducted on 40 mice divided into 2×2 groups. Researchers fed one group of mice a regular diet while adding steamed broccoli sprouts to the other group’s diet. Researchers chemically induced bowel inflammation (colitis) in one-half of the mice from each group, while the other half did not undergo this induction. In that way, there were four groups, with ten mice in each – the group fed a regular diet with induced colitis, the group fed a regular diet without induced colitis, the group fed a diet with broccoli sprouts without induced colitis, and the group fed a diet with broccoli sprouts with induced colitis. The study started when the mice were seven weeks old and continued for 34 days.
Researchers prepared the broccoli sprouts for 10 minutes in a double boiler. They then cooled the steamed broccoli sprouts down and stored them in a -80oC freezer until they freeze-dried. Researchers then ground the freeze-dried broccoli sprouts into a fine powder and added the powder to the regular mice food, constituting 10% of the food by weight (see Figure 3.1).
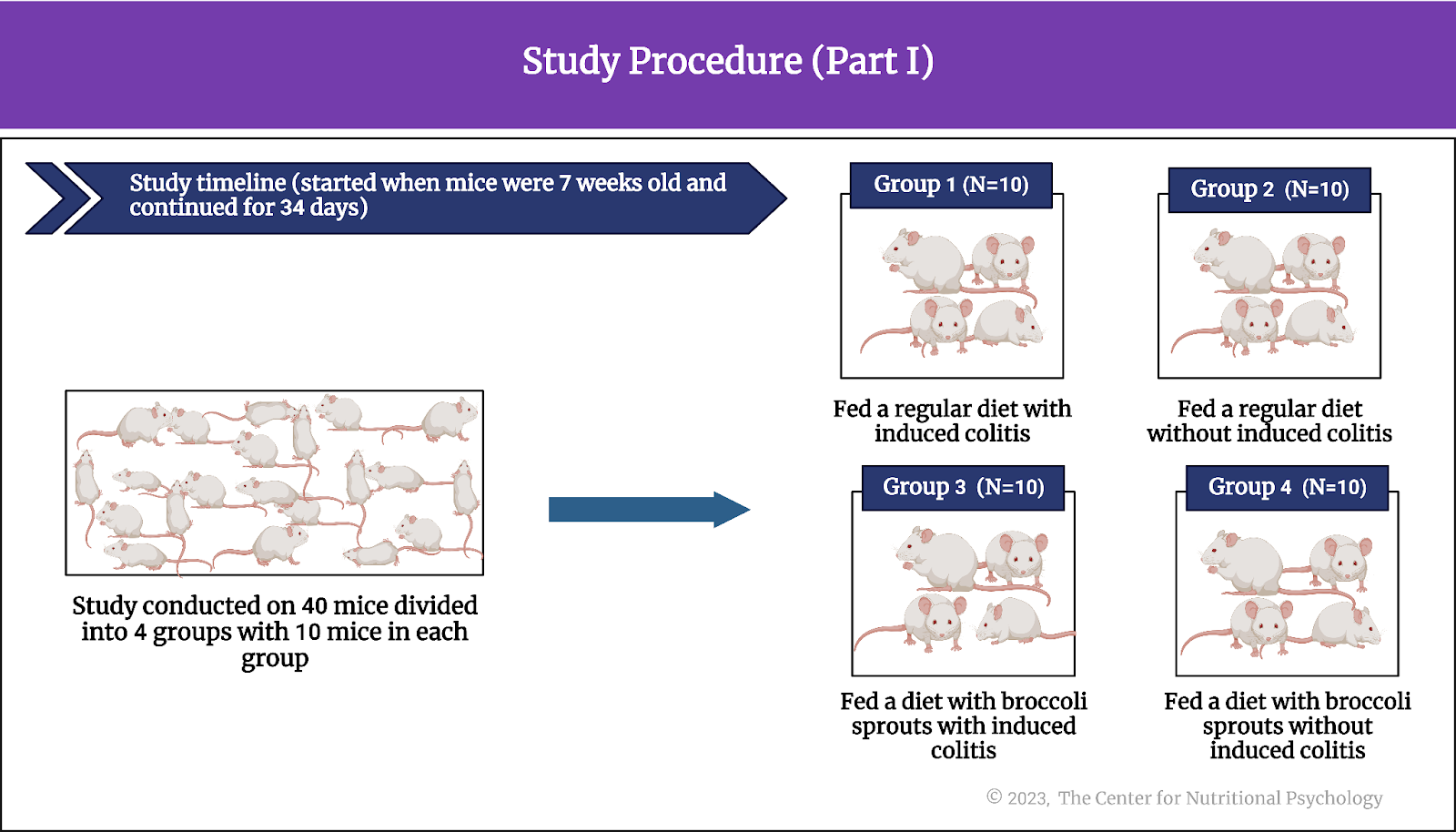
Figure 3.1. Study Procedure (Part I)
Dextran sodium sulfate (DSS) in water
The study authors added dextran sodium sulfate (DSS) to the water two groups (group I & group 3) of mice drank to induce colitis. When consumed, dextran sodium sulfate disrupts the expression of certain proteins in the cells lining the intestines. This disruption causes the cells lining the intestine walls to become permeable, leading to a leaky barrier. The leakiness of this barrier triggers a host of events that result in inflammation and symptoms similar to colitis in humans.
Researchers started putting dextran sodium sulfate in the water the mice drank starting from the 7th day of the study. Its concentration in water was 2.5%. They gave mice water with dextran sodium sulfate for five days. This was followed by a recovery period of 5-7 days (no dextran sodium sulfate in water), after which they repeated the procedure. There were three cycles during which water with dextran sodium sulfate was given to mice (Figure 3.2).
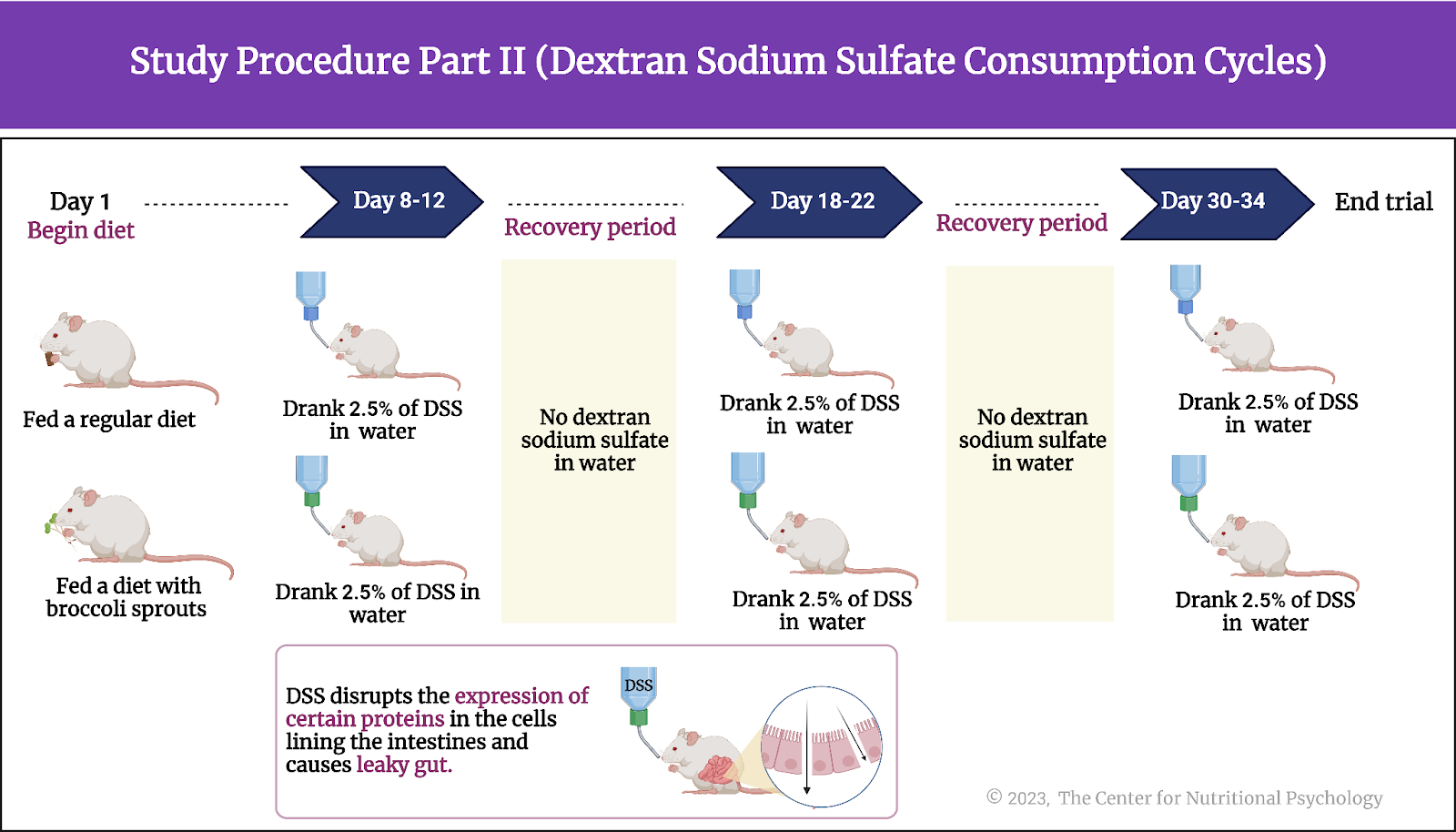
Figure 3.2. Study procedure Part II (Dextran sodium sulfate consumption cycles)
Assessments
The study authors assessed the severity of symptoms caused by the treatment through a combination of factors, including the mice’s body weight, fecal consistency, and the presence of blood in feces. They collected fecal samples of these mice every 2-3 days and every day during periods when mice drank water with dextran sodium sulfate.
After the study period, mice were euthanized, and researchers studied gut microbiota contents in various places in mice’s digestive tracts using genetic techniques. They also determined various inflammation indicators (cytokines) levels from their blood (see Figure 4).
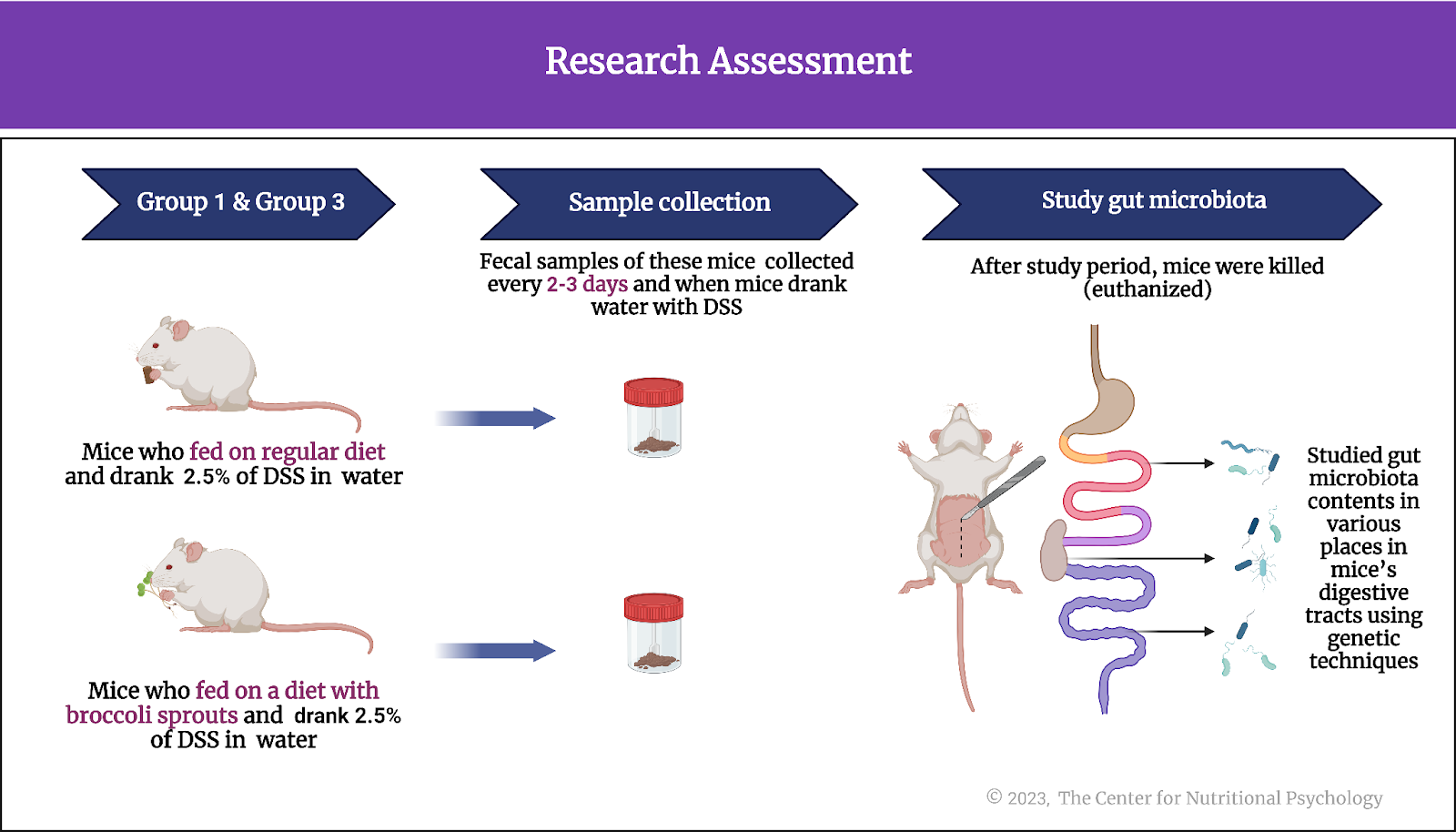
Figure 4. Research Assessment
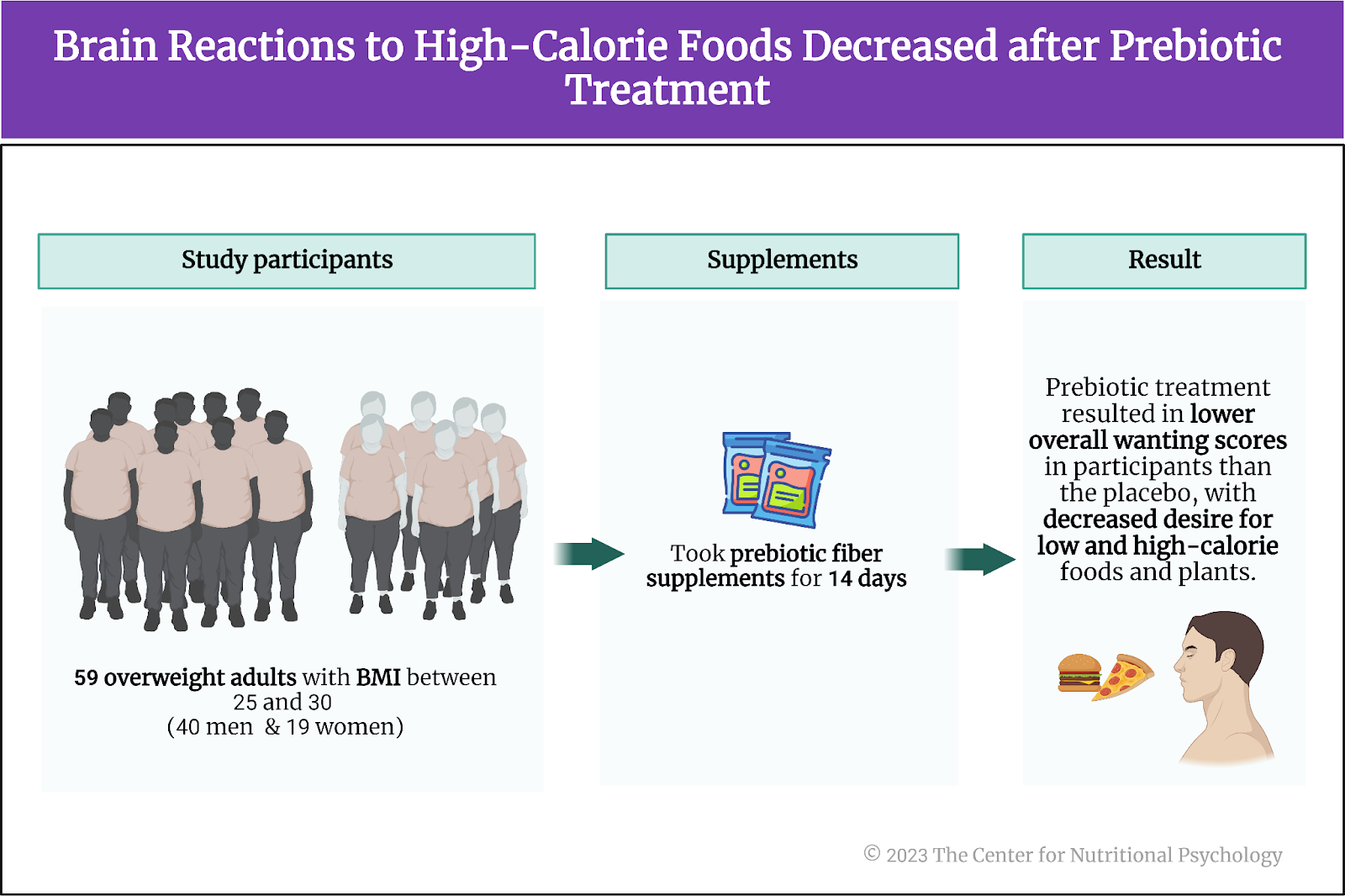
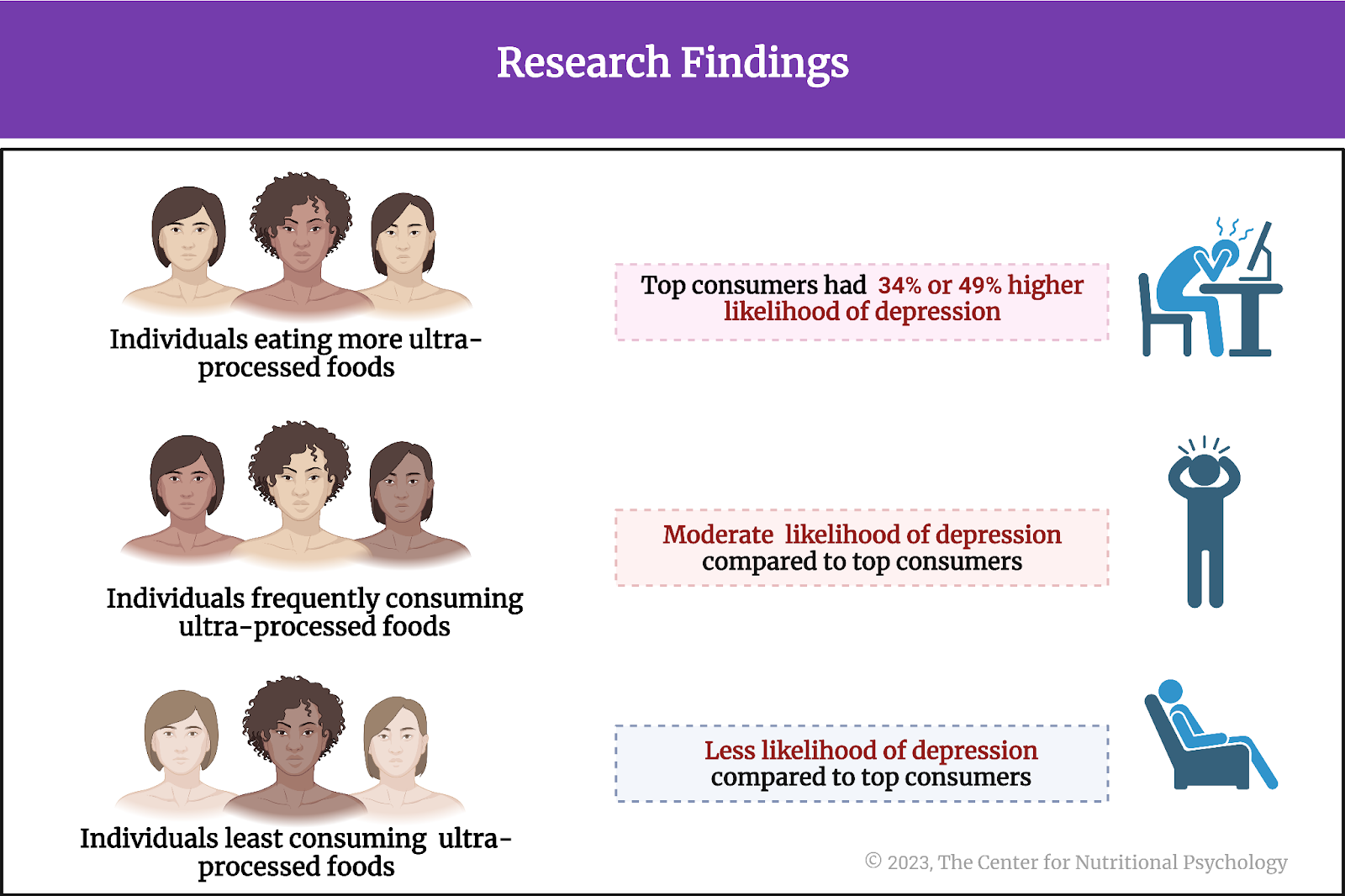
Broccoli sprouts alleviated the symptoms of colitis
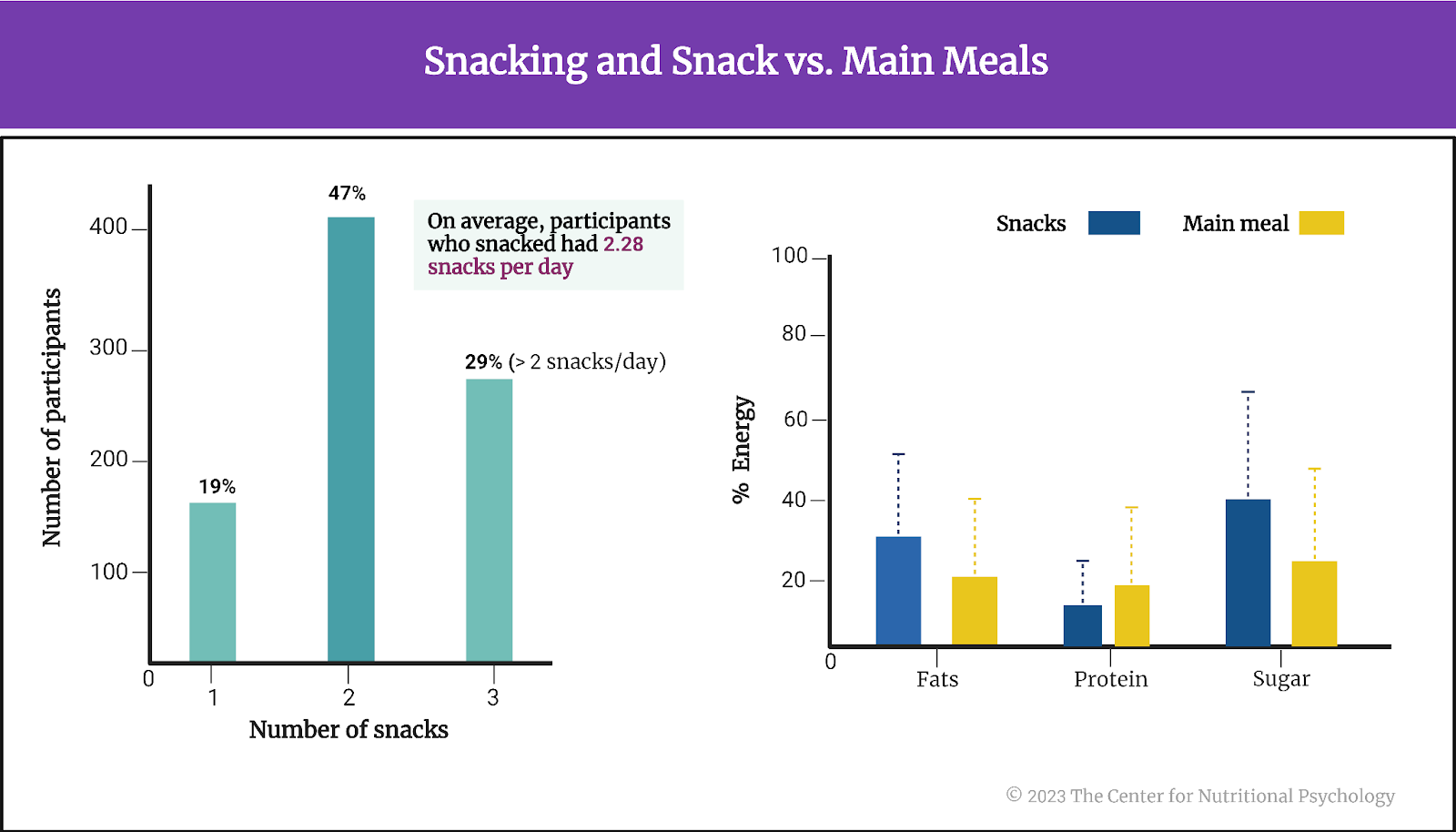
Results showed that, during the study period, mice with induced colitis who ate a diet with broccoli sprouts gained more weight than mice with induced colitis on the regular diet. Although mice were still in their growth phase and expected to gain weight naturally, the first two cycles of dextran sodium sulfate treatments led to weight loss. However, mice on the broccoli sprout diet regained the lost weight by the beginning of the next cycle, while mice on the regular diet did not. At the end of the study, mice fed a regular diet with induced colitis had the lowest weight of all groups.
Mice with induced colitis who were fed a diet with broccoli sprouts had less pronounced symptoms of colitis and lower levels of some of the inflammation markers (proinflammatory cytokines IL-1 beta, IL-6, and tumor necrosis factor-alpha (TNF-α) compared to mice with induced colitis on the regular diet (see Figure 5).
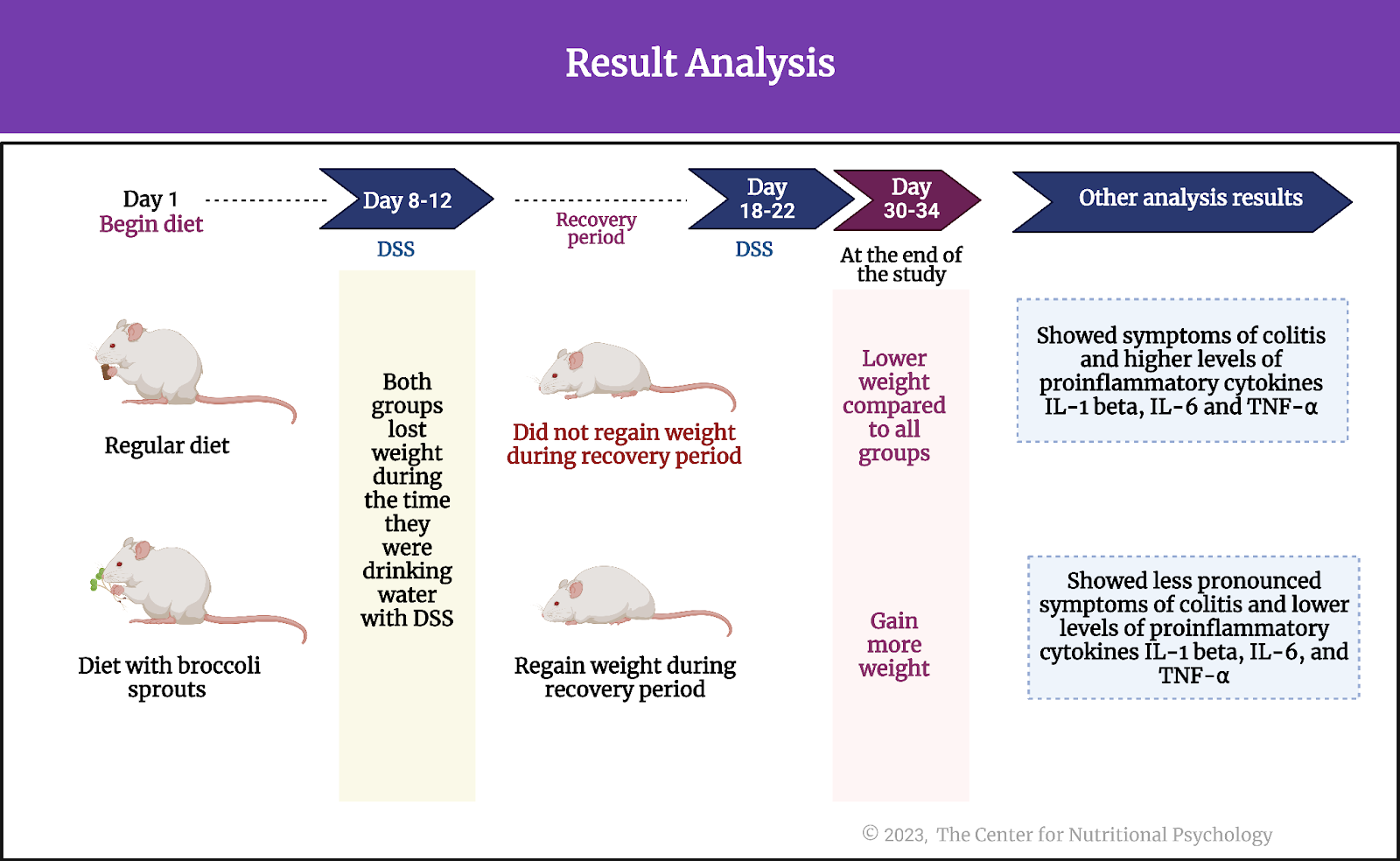
Figure 5. Result analysis (Holman et al., 2023)
Broccoli sprouts protected against changed to bacterial community induced by colitis
Mice on a broccoli sprout diet with induced colitis had significantly more bacterial richness in their colon contents and on the colon walls (materials scraped from the colon) compared to mice with induced colitis on the regular diet. Comparing all four groups, results showed that the two groups that consumed diets with broccoli sprouts had higher bacterial richness in all gut locations, with the most notable difference observed in the colon.
Further analysis showed that the gut bacterial community of mice with induced colitis that consumed a diet with broccoli sprouts differed in which bacterial species were present from those of mice with induced colitis that consumed the regular diet. This indicated that broccoli sprouts strongly protected against changes to bacterial communities induced by dextran sodium sulfate.
Conclusion
Overall, the study results show that adding steamed broccoli sprouts to the diet of mice alleviates the effects of chemically induced bowel inflammation – colitis, but also protects microbial communities in their guts from changes induced by the treatment designed to induce colitis. Bacterial richness in various locations in the gut was similar between mice with induced colitis consuming broccoli sprouts and mice without colitis on a regular diet.
Although these findings were obtained on mice using chemically induced bowel inflammation, similarities with human biochemistry and inflammatory bowel diseases might be sufficient for similar effects. Since broccoli sprouts are widely available and affordable food items, adding them to a diet might be an easily implementable way to reduce symptoms of inflammatory bowel diseases and protect the gut microbiome. Of course, further study is needed to confirm that the effects observed in this study would also be present in humans with inflammatory bowel diseases. However, adding broccoli sprouts to the diet is a promising strategy.
Since broccoli sprouts are widely available and affordable food items, adding them to a diet might be an easily implementable way to reduce symptoms of inflammatory bowel diseases and protect the gut microbiome
The paper “Steamed broccoli sprouts alleviate DSS-induced inflammation and retain gut microbial biogeography in mice” was authored by Johanna M. Holman, Louisa Colucci, Dorien Baudewyns, Joe Balkan, Timothy Hunt, Benjamin Hunt, Marissa Kinney, Lola Holcomb, Allesandra Stratigakis, Grace Chen, Peter L. Moses, Gary M. Mawe, Tao Zhang, Yanyan Li, and Suzanne L. Ishaq.
References
Carbia, C., Bastiaanssen, T. F. S., Iannone, F., García-cabrerizo, R., Boscaini, S., Berding, K., Strain, C. R., Clarke, G., Stanton, C., Dinan, T. G., & Cryan, J. F. (2023). The Microbiome-Gut-Brain axis regulates social cognition & craving in young binge drinkers. EBioMedicine, (In press), 104442. https://doi.org/10.1016/j.ebiom.2023.104442
Holman, J. M., Colucci, L., Baudewyns, D., Balkan, J., Hunt, T., Hunt, B., Kinney, M., Holcomb, L., Stratigakis, A., Chen, G., Moses, P. L., Mawe, G. M., Zhang, T., Li, Y., & Ishaq, S. L. (2023). Steamed broccoli sprouts alleviate DSS-induced inflammation and retain gut microbial biogeography in mice. MSystems. https://doi.org/10.1128/msystems.00532-23
Leclercq, S., Le Roy, T., Furgiuele, S., Coste, V., Bindels, L. B., Leyrolle, Q., Neyrinck, A. M., Quoilin, C., Amadieu, C., Petit, G., Dricot, L., Tagliatti, V., Cani, P. D., Verbeke, K., Colet, J. M., Stärkel, P., de Timary, P., & Delzenne, N. M. (2020). Gut Microbiota-Induced Changes in β-Hydroxybutyrate Metabolism Are Linked to Altered Sociability and Depression in Alcohol Use Disorder. Cell Reports, 33(2). https://doi.org/10.1016/J.CELREP.2020.108238
Ng, S. C., Shi, H. Y., Hamidi, N., Underwood, F. E., Tang, W., Benchimol, E. I., Pannacione, R., Ghosh, S., Wu, J. C. Y., Chan, F. K. L., Sung, J. J. Y., & Kaplan, G. G. (2017). Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. The Lancet, 390(10114), 2769–2778.
Ramos, G. P., & Papadakis, K. A. (2019). Mechanisms of Disease: Inflammatory Bowel Diseases. Mayo Clinic Proceedings, 94(1), 155–165. https://doi.org/10.1016/j.mayocp.2018.09.013
Tilg, H. (2015). Cruciferous vegetables: prototypic anti-inflammatory food components. Tilg Clinical Phytoscience, 1(10). https://doi.org/10.1186/s40816-015-0011-2