- A meta-analysis published in BMC Psychiatry found that individuals consuming junk food frequently had 16% higher odds of having depression and 33% higher odds of experiencing increased stress.
- Junk food consumption was also associated with 15% higher odds of developing mental health problems in general.
- The meta-analysis included 17 studies with a total of 159,885 participants.
We all know that preparing nutritious and healthy meals can sometimes require quite a bit of work. We need to buy all the groceries, spend time cleaning and cutting them, cook them using various methods, season them, and finally serve them as a dish. This work becomes more challenging when we are ill, overworked, or not feeling well for various reasons. In such situations, many consider affordable, ready-made food or food that can be prepared for eating with minimal effort (e.g., by simply heating it) to be a good alternative, given its alluring taste. However, many such food items available in the market are junk food.
Junk food
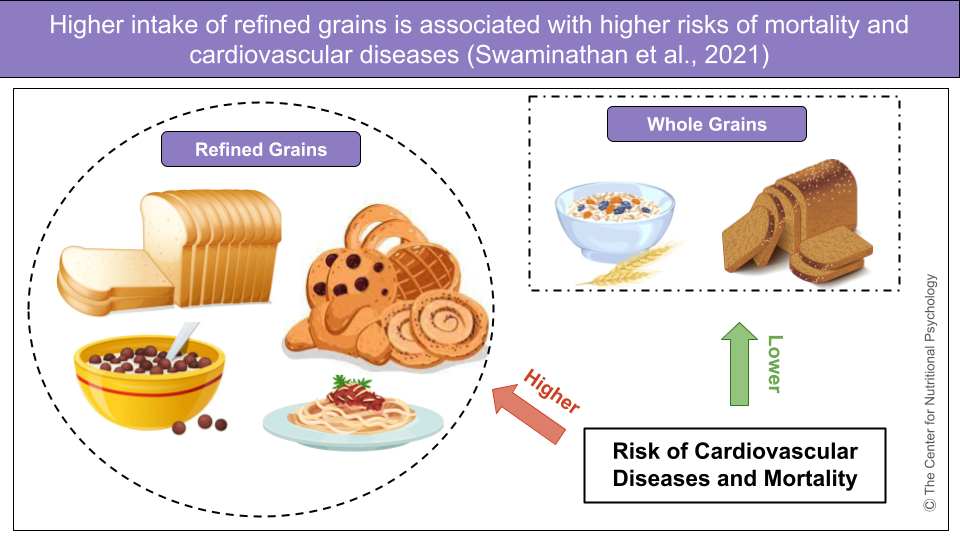
“Junk food” (Hedrih, 2025) is food that is high in calories, sugar, salt, and unhealthy fats, but low in essential nutrients like fiber, vitamins, and minerals. It includes ultraprocessed foods, fast foods, unhealthy snacks, and sugar-sweetened beverages (Ejtahed et al., 2024). Ultraprocessed foods, a subcategory of junk foods, are industrially manufactured products made from refined ingredients, additives, and preservatives, with little to no whole food content. They are primarily designed for convenience and long shelf life (Hedrih, 2023, 2024a). Examples of junk Food include chips, candy, soda, fast food burgers, and pre-fried snacks (see Figure 1).

Figure 1. Characterization of the term “junk food” used in research
Regular consumption of junk food is linked to obesity, type 2 diabetes, heart disease, and other chronic health conditions (Rajveer & Monika, 2012). These foods tend to be heavily processed and designed to be hyper-palatable, making them easy to overeat. Junk food is widely marketed, especially to children and adolescents, contributing to unhealthy eating habits (Harris & Graff, 2012).
Junk food and health
In recent decades, scientists have been paying increased attention to the relationship between food, eating habits, and health. The world is currently going through an obesity pandemic (Wong et al., 2022), with the percentage of overweight and obese individuals in double digits in most countries. Unlike in previous centuries, when humans struggled to produce enough calories for everyone and avoid recurring famines, modern human society’s challenge is maintaining food intake regulation that supports good health.
Studies have so far shown that a diet based on foods rich in easily digestible fats and sugar (such as junk food) can dysregulate the food intake regulation mechanisms in our brains, leading to obesity (Hedrih, 2024b; McDougle et al., 2024). This mechanism is well-known in studies on rodents, where such a diet is referred to as an obesogenic diet and is used to experimentally induce obesity (Ikemoto et al., 1996).
The world is currently going through an obesity pandemic
(Wong et al., 2022).
Some researchers propose that humans can develop patterns of behavior around food similar to those found in substance use disorders. They refer to it as food addiction, suggesting that ultraprocessed foods, along with additives found in such foods, lead to this addiction (Gearhardt et al., 2023; Hedrih, 2023).
Unlike in previous centuries, the primary challenge for modern human society is maintaining food intake regulation.
The current study
Study author Hanieh-Sadat Ejtahed wanted to integrate the findings of published scientific studies on the links between junk food consumption and mental health disorders in adults (Ejtahed et al., 2024). They conducted a systematic review and a meta-analysis.
These authors searched the databases of scientific publications PubMed/ Medline, ISI Web of Science, Scopus, Cochrane, Google Scholar, and EMBASE up to July 2023. They used keywords like “sweetened drink” or “sweetened beverage”, “processed food”, “junk food”, “fried food”, “instant food”, and several others, along with keywords for mental health conditions and concepts such as “sleep disorders”, “mental health”, “depression”, “stress”, “happiness”, and “well-being”. They sought scientific publications reporting the associations between junk food consumption and mental health.
The search initially returned 1745 records. However, after removing duplicates, publications that were not relevant to the study goal, and studies on children (the authors were interested in adults), the number of studies was reduced to 17. They involved 159,885 participants.
Junk food consumption is associated with a 15% increased risk of having depression
Analysis of these studies showed that all of them reported at least one link between junk food consumption and adverse psychological outcomes. Integration of results of 4 studies on stress suggested that individuals consuming high levels of junk food have 33% higher odds of being under increased stress. Junk food consumption was associated with 15% higher odds of mental health issues in general.
An analysis of studies looking into links with depression indicated that frequent junk food consumption was associated with 15% increased odds of depression (compared to individuals not consuming junk food or consuming it much less).
However, findings reported by various studies tended to be quite diverse. For example, studies looking into the links between depression and junk food consumption reported increased odds of depression for individuals consuming lots of junk food, ranging from 3% higher to 77% higher. Similarly, increased odds reported by cross-sectional studies looking into links between junk food and stress ranged from 5% higher to 73% higher (see Figure 2).

Figure 2. Procedure and findings (Ejtahed, 2024)
Conclusion
The study results indicate that frequent consumption of junk food, i.e., foods high in fat and sugar content and low in nutritive value, is associated with poorer mental health. This might mean that a diet based on junk food adversely affects mental health, but it could also mean that individuals in poor mental health, dealing with depression and increased stress, are less able to provide themselves with a healthy diet.
Future studies are needed to explore the mechanisms behind this relationship. However, the existence of this link indicates that interventions aimed at supporting mental health or treating mental health issues need to consider their patients’ nutrition habits and nutrition options.
The paper “Association between junk food consumption and mental health problems in adults: a systematic review and meta-analysis” was authored by Hanieh-Sadat Ejtahed, Parham Mardi, Bahram Hejrani, Fatemeh Sadat Mahdavi, Behnaz Ghoreshi, Kimia Gohari, Motahar Heidari-Beni, and Mostafa Qorbani.
References
Ejtahed, H.-S., Mardi, P., Hejrani, B., Mahdavi, F. S., Ghoreshi, B., Gohari, K., Heidari-Beni, M., & Qorbani, M. (2024). Association between junk food consumption and mental health problems in adults: A systematic review and meta-analysis. BMC Psychiatry, 24(1), 438. https://doi.org/10.1186/s12888-024-05889-8
Gearhardt, A. N., Bueno, N. B., DiFeliceantonio, A. G., Roberto, C. A., Jiménez-Murcia, S., & Fernandez-Aranda, F. (2023). Social, clinical, and policy implications of ultra-processed food addiction. BMJ, e075354. https://doi.org/10.1136/bmj-2023-075354
Harris, J. L., & Graff, S. K. (2012). Protecting Young People From Junk Food Advertising: Implications of Psychological Research for First Amendment Law. American Journal of Public Health, 102(2), 214–222. https://doi.org/10.2105/AJPH.2011.300328
Hedrih, V. (2023). Scientists Propose that Ultra-Processed Foods be Classified as Addictive Substances. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/scientists-propose-that-ultra-processed-foods-be-classified-as-addictive-substances/
Hedrih, V. (2024a). What are Ultra-Processed Foods Doing to Your Mental and Physical Health? CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/what-are-ultra-processed-foods-doing-to-your-mental-and-physical-health/
Hedrih, V. (2024b, February 19). Consuming Fat and Sugar (At The Same Time) Promotes Overeating, Study Finds. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/16563-2/
Hedrih, V. (2025). Does Eating Lots of Junk Food Lead to Poor Mental Health? CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/does-eating-lots-of-junk-food-lead-to-poor-mental-health/
Ikemoto, S., Takahashi, M., Tsunoda, N., Maruyama, K., Itakura, H., & Ezaki, O. (1996). High-fat diet-induced hyperglycemia and obesity in mice: Differential effects of dietary oils. Metabolism, 45(12), 1539–1546. https://doi.org/10.1016/S0026-0495(96)90185-7
McDougle, M., de Araujo, A., Singh, A., Yang, M., Braga, I., Paille, V., Mendez-Hernandez, R., Vergara, M., Woodie, L. N., Gour, A., Sharma, A., Urs, N., Warren, B., & de Lartigue, G. (2024). Separate gut-brain circuits for fat and sugar reinforcement combine to promote overeating. Cell Metabolism. https://doi.org/10.1016/j.cmet.2023.12.014
Rajveer, B., & Monika, O. (2012). Junk Food: Impact on health. Journal of Drug Delivery & Therapeutics, 2(3), 67–73.
Wong, M. C., Mccarthy, C., Fearnbach, N., Yang, S., Shepherd, J., & Heymsfield, S. B. (2022). Emergence of the obesity epidemic: 6-decade visualization with humanoid avatars. The American Journal of Clinical Nutrition, 115(4), 1189–1193. https://doi.org/10.1093/AJCN/NQAC005