Consuming Fat and Sugar (At The Same Time) Promotes Overeating, Study Finds
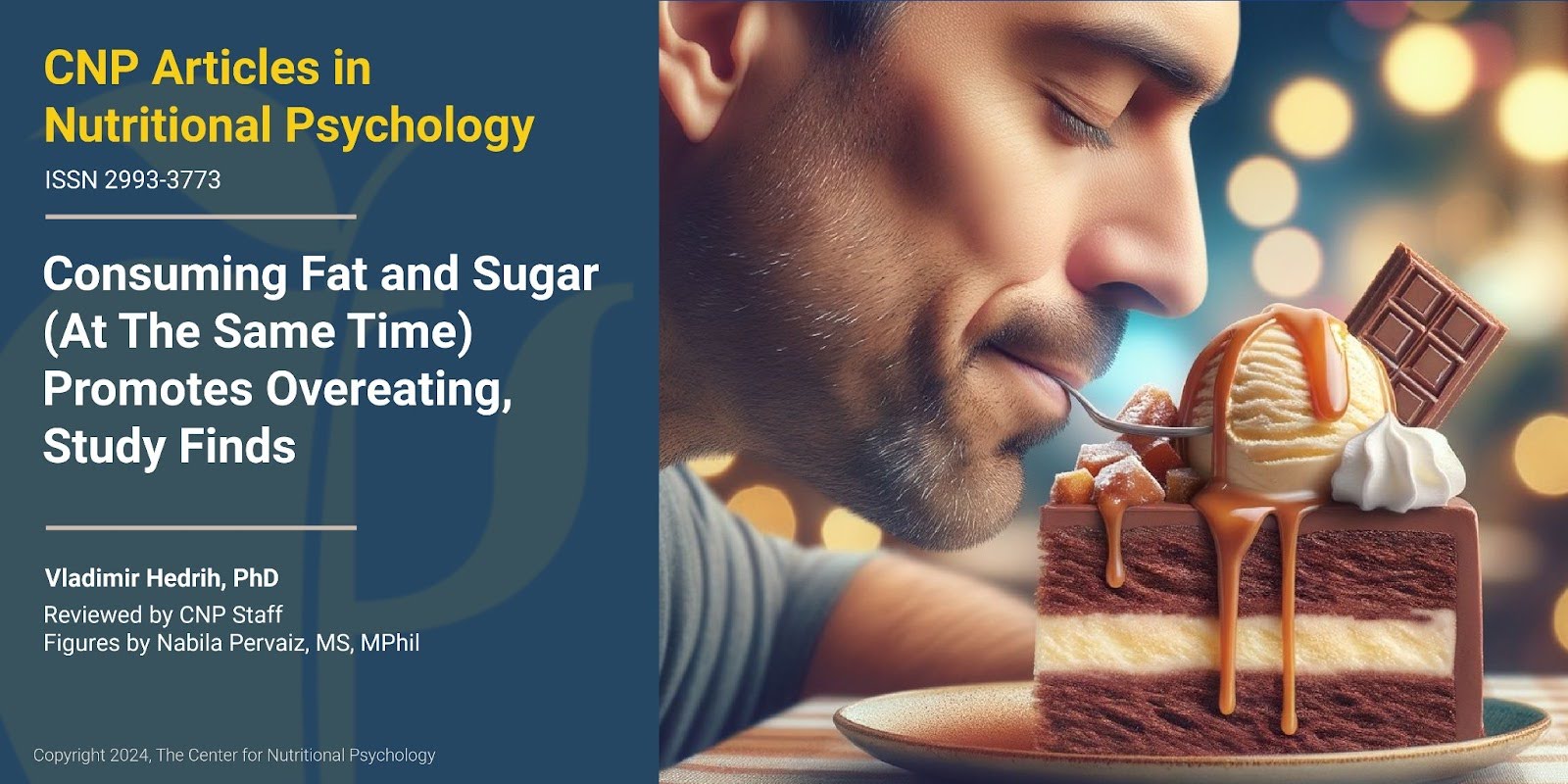
Listen to this Article
- A study on mice published in Cell Metabolism found that gut-brain neural circuits conveying and processing information about the presence of fat and sugar in the gut are separate
- Foods that contain both sugar and fats activate both circuits, releasing more dopamine compared to foods of equal caloric value containing only fat
- The large amounts of dopamine released in this way create feelings of pleasure that promote overeating on the types of food that caused the release
When we want to find out what a piece of food is like, we can taste or smell it. When we smell something, sensory cells located in a small patch of tissue (olfactory epithelium) at the top of our nasal cavity react to the odorant molecules coming from that piece of food, and the olfactory nerve to carries the information to our brain, allowing us to experience smell. Similarly, when we taste a piece of food, taste buds in our mouth react to it, and specific nerves carry the information to our brain. While we eat, this evaluation of the qualities of food using our sensory organs happens continuously. However, not all of our food sensations come from our external senses. Our body also has sensory cells in the gut that inform the brain about what we eat.
The vagus nerve
After we ingest food through our mouth, it enters the esophagus. It continues towards the stomach and, after that, into the intestine. Food is further digested and broken down into components absorbed into the body as nutrients in these parts of the gastrointestinal system.
There are sensory cells located throughout the gastrointestinal system. The vagus nerve, one of the longest nerves in the body, connects these cells to the brain through a communication pathway called the gut-brain axis. In this way, it conveys sensory information about the state of the intestinal environment, including nutrient levels, gut microbiota activity, and intestinal wall integrity from the gut to the brain. These signals are then integrated into the brainstem, allowing the brain to monitor and respond to gut activity, influencing digestive processes, immune responses, and emotional states. (Bonaz et al., 2018) (see Figure 1).
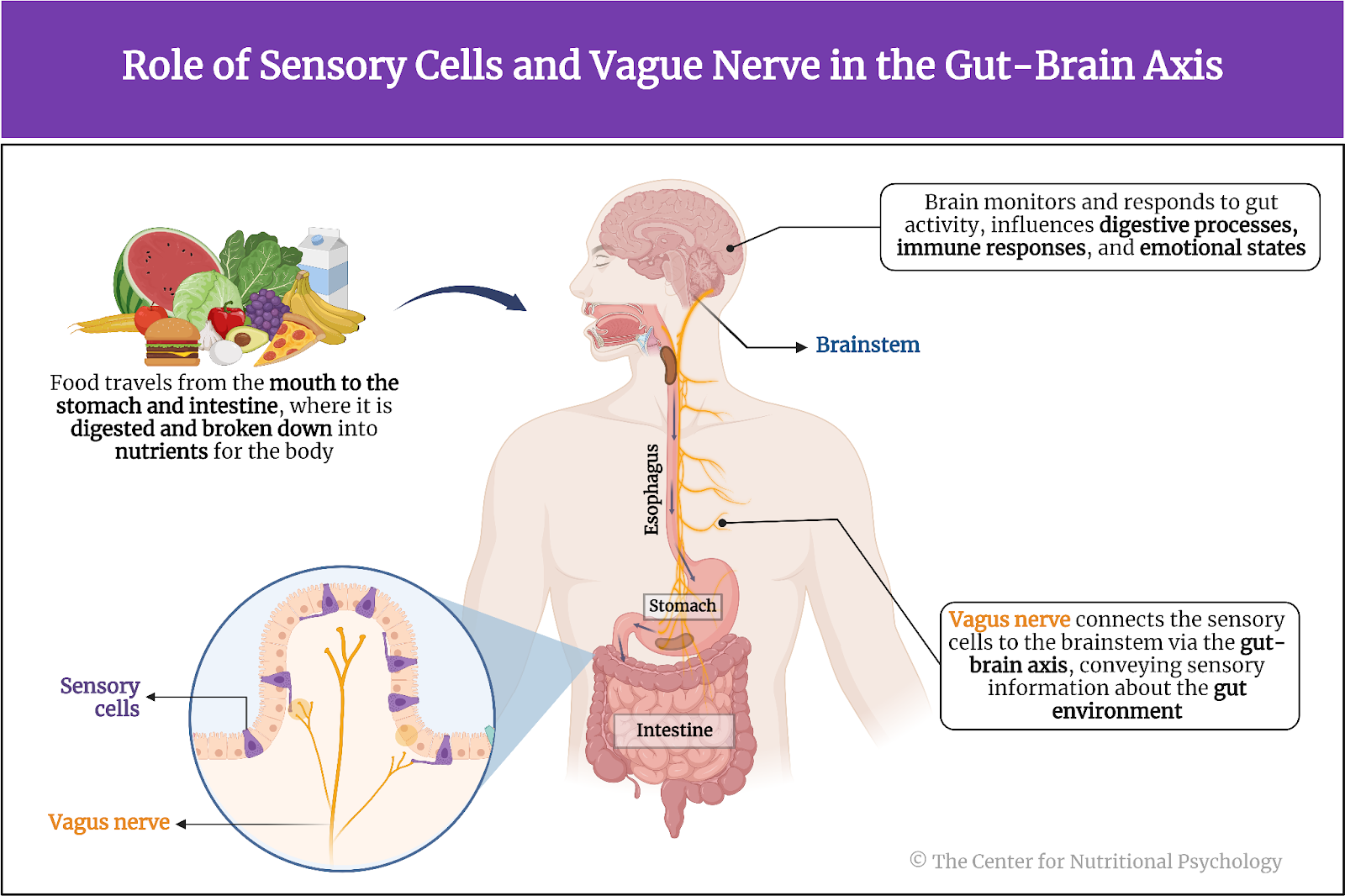
Figure 1. Role of sensory cells and vagus nerve in the Gut-Brain Axis.
Among other things, the vagus nerve carries information to the brain about the nutritional value of our food. However, scientists so far have not fully understood the intricate details of how this system functions (McDougle et al., 2024).
The obesity pandemic
Recent decades have seen a continued increase in the share of obese individuals throughout the developed world. Many call this the obesity pandemic (Wong et al., 2022). This has motivated many studies into the causes of this pandemic. Results point to an intricate interplay between specific types of nutrients and other substances in the food and the properties of the human central nervous system as important contributing causes of obesity (Wilding, 2001).
Notably, while human brains (and brains of many other species) have a food intake regulation mechanism that determines when we will feel a desire to eat or when we will feel satiated, studies indicate that parts of this mechanism might be malfunctioning in obese individuals (Pujol et al., 2021; Seabrook et al., 2023). Studies indicate that feeding rodents high-fat diets instead of their regular chow can, in time, dysregulate their food intake regulation mechanisms, leading them to eat more calories than they need, resulting in obesity (Ikemoto et al., 1996). In humans, studies have linked the dysregulation of this mechanism with the consumption of foods that are both fatty and sweet (a property rarely found in natural foods) but also to various additives that create addiction-like reactions to foods that contain them (Hedrih, 2023).
The current study
Study author Molly McDougle and her colleagues wanted to explore the neural pathways through which the brain detects the intake of fats and sugars (i.e., fatty and sweet foods). They wanted to know whether the intake of these two types of nutrients triggers the same sensory neurons and whether they engage overlapping or separate neural circuits.
What was known before this study was that a direct infusion of fats or sugars into the gut (of mice) activates the vagus nerve. This, in turn, leads to the release of the neurotransmitter dopamine in the dorsal striatum region of the brain. The dorsal striatum is involved in reward and motivation processing, and dopamine is a key neurotransmitter that signals pleasure and reward (see Figure 2).
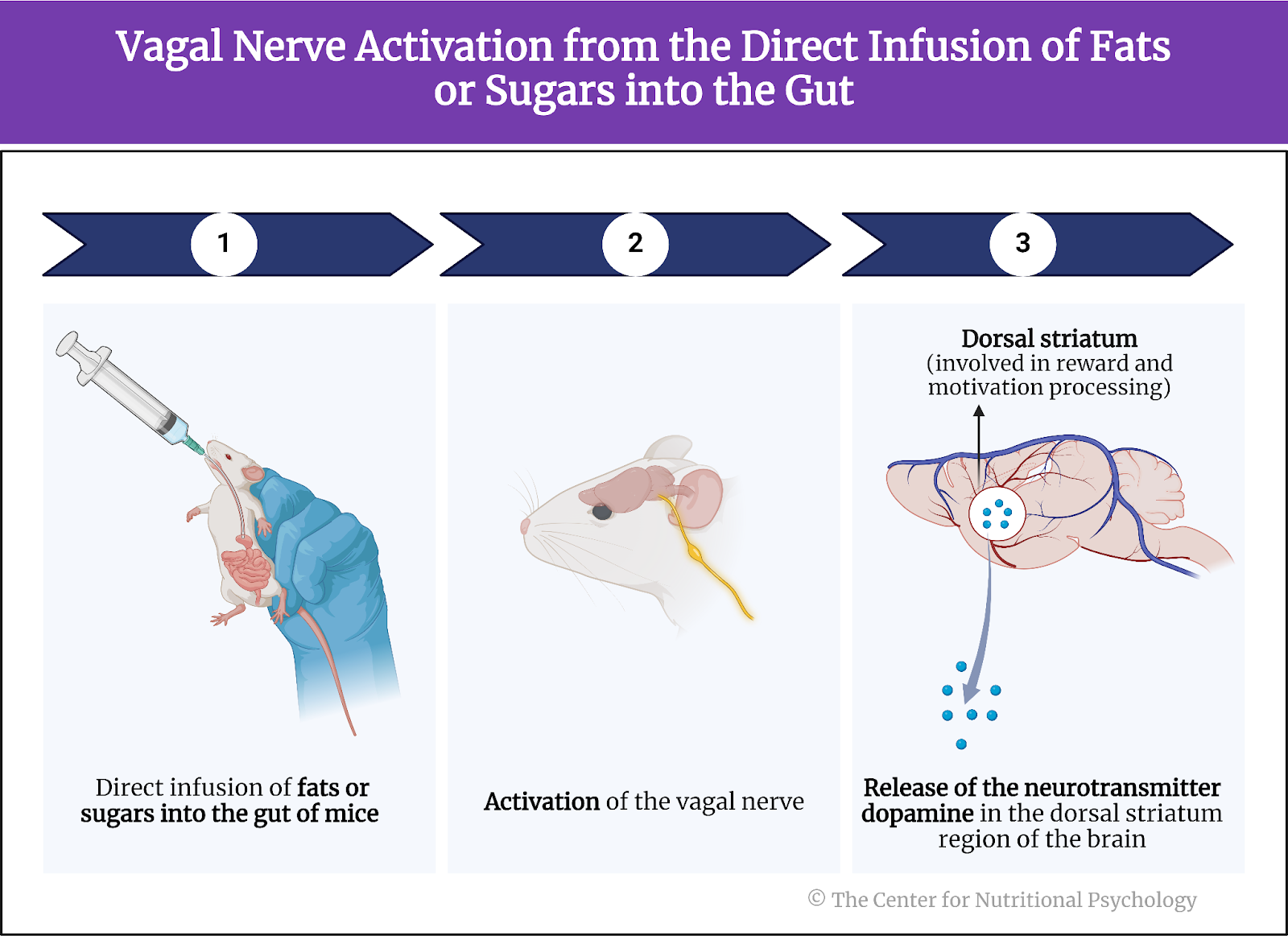
Figure 2. Vagal nerve activation from the direct infusion of fats or sugars into the gut
Study procedure
The study was conducted on 70 mice. The mice used in this study were between 6 and 20 weeks of age. Thirty-five mice were male, and 35 were female. They were housed at 22 degrees C and had free access to mouse food.
The study authors performed a series of experiments on these mice. The experiments involved surgical procedures that exposed or cut the vagus nerve and/or exposed the nodose ganglion (a part of the vagus nerve) for further activities. These surgeries also involved the implantation of catheters that allowed researchers to inject fluids directly into the gut of these mice, bypassing the mouth and, thus, taste receptors.
These researchers used 2-photon imaging to study the activity of the nodose ganglion in the mice (while the mice were alive) and of brain areas involved in sensing and processing information about nutrient intake. Two-photon imaging is a fluorescence microscopy technique that allows for deep-tissue, high-resolution imaging of live cells and tissues. It uses two photons of lower energy to excite a fluorophore simultaneously. Fluorophores are special molecules that emit a visible glow when excited by light of a specific wavelength, thus allowing researchers to track and observe different biological processes or structures.
Other experimental procedures included behavioral tests, techniques using light to control neurons that have been genetically modified to express ion channels sensitive to light (optogenetics), sampling extracellular fluid from the dorsal striatum region of the brain to measure the quantities of dopamine (microdialysis) and others. In the end, the study authors harvested and analyzed the brain tissues of these mice (see Figure 3).
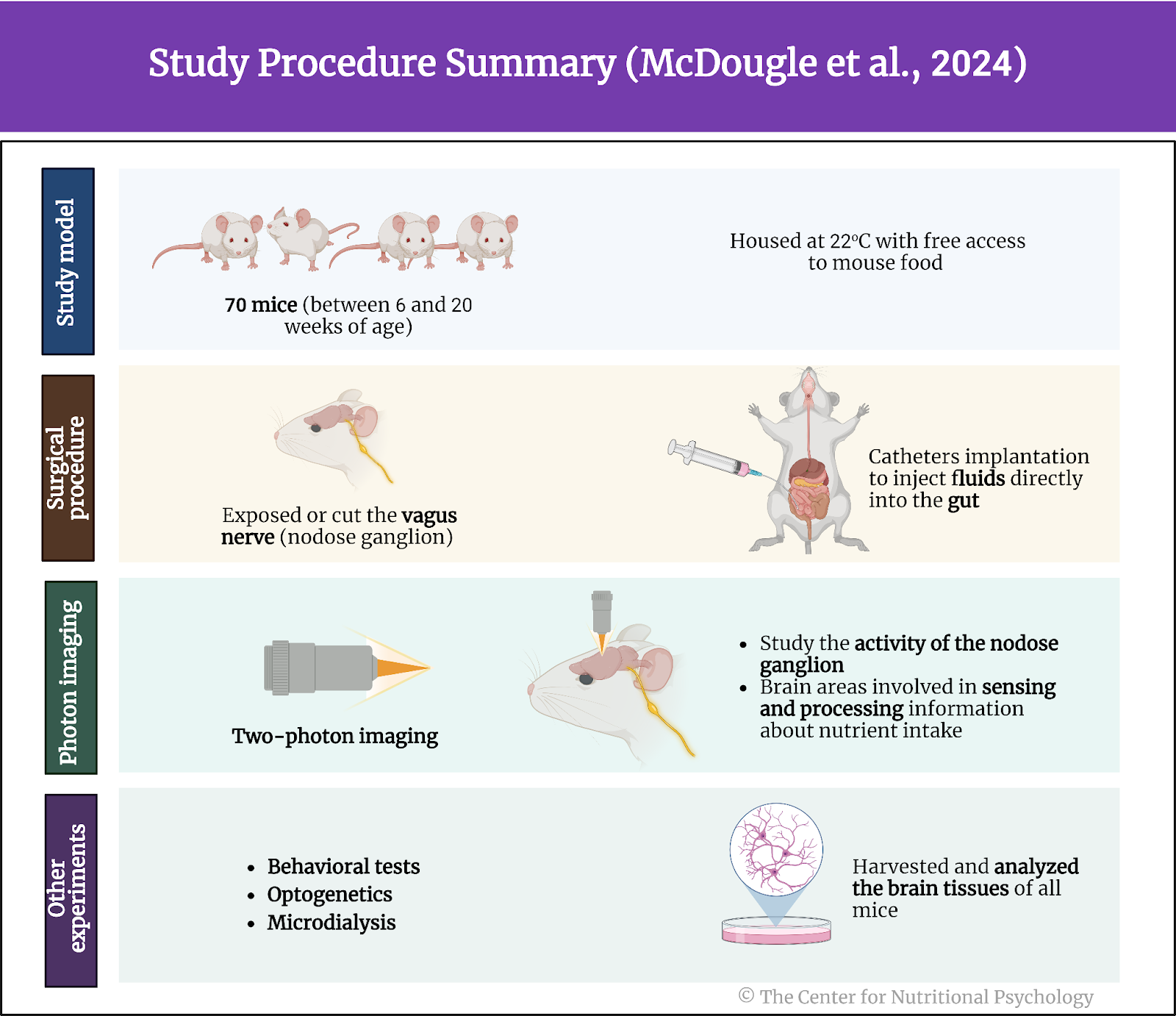
Figure 3. Study procedure summary (McDougle et al., 2024).
Fats and sugars are sensed by separate neurons of the vagal nerve
Results showed that fats and sugars increased the activity of neurons in the vagus nerve, but mostly not of the same ones. Neurons comprising the nodose ganglion mostly reacted to the presence of fat or sugars. Very few neurons reacted to both. These neurons reacting to nutrients in the intestine comprised around 17% of the neurons in the nodose ganglion. The nodose ganglion is a cluster of sensory neurons located on the vagus nerve, transmitting visceral sensory information from the body to the brain.
When researchers infused sugar or fat into the guts of mice, the neurons of the nodose ganglion they previously marked increased their frequencies of nerve impulses. Analysis of the neural circuits activated by fats and sugars showed that they differ. They were largely separate. Information about sugar and fats in the gut is carried to the brain through two distinct pathways. These pathways convey information about the type of nutrient in the gut, but they also likely convey information about its concentration (see Figure 4).
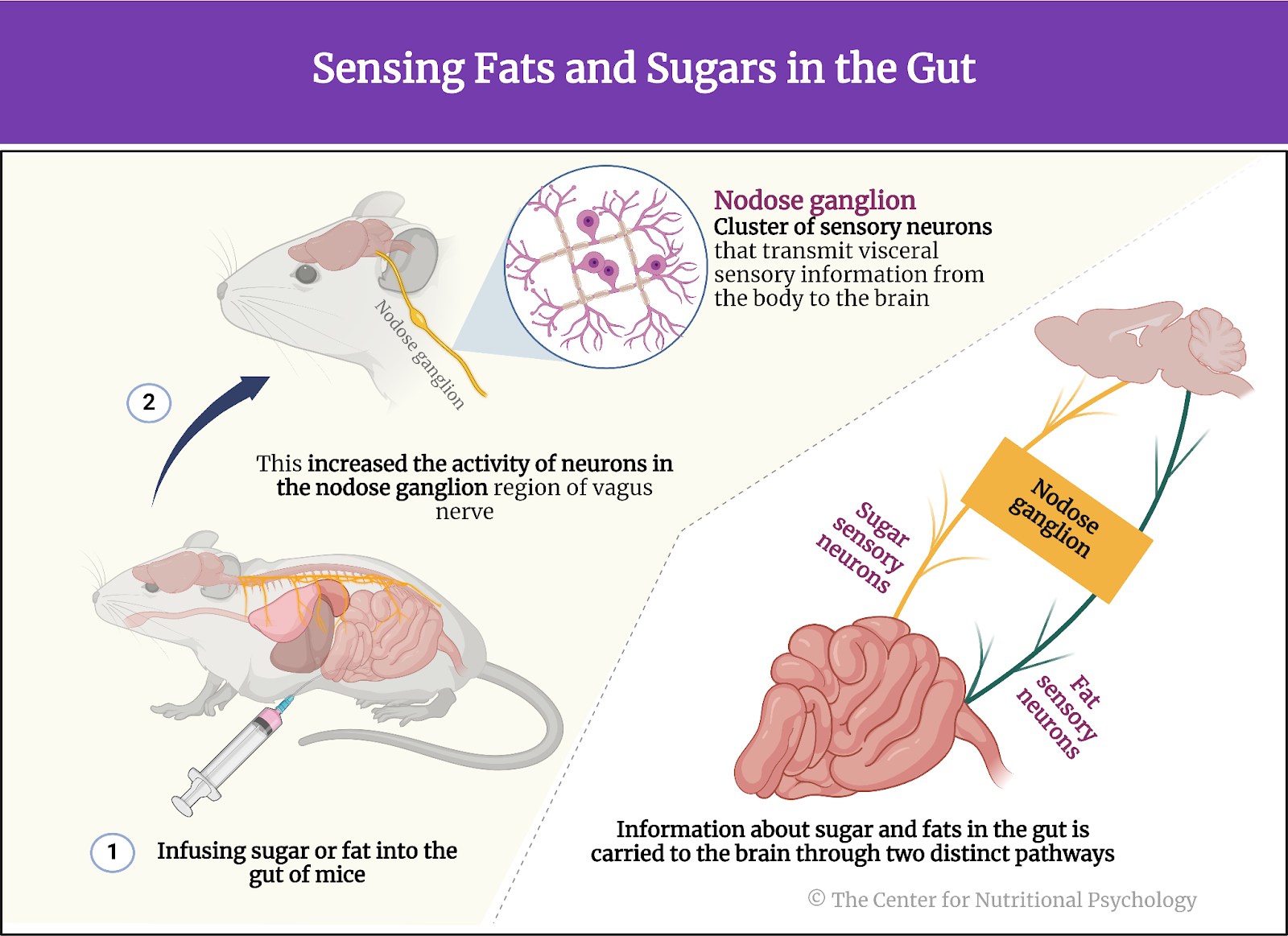
Figure 4. Sensing fats and sugars in the gut
The duodenum is the key sensing site for both sugar and fat
Tracing the locations of sensory cells, these neurons led these researchers to discover an extensive network of sensory cells in the duodenum. Almost all sensory cells detecting fats and many of those detecting sugars were located there. The duodenum is the first section of the small intestine, connecting the stomach to the jejunum. It plays a crucial role in the initial phase of digestion by receiving partially digested food from the stomach and digestive enzymes from the pancreas and liver. On the other hand, study authors found that sugar-sensing also happens in the hepatic portal vein, a blood vessel that carries nutrient-rich blood from the gastrointestinal tract and spleen to the liver (see Figure 5).
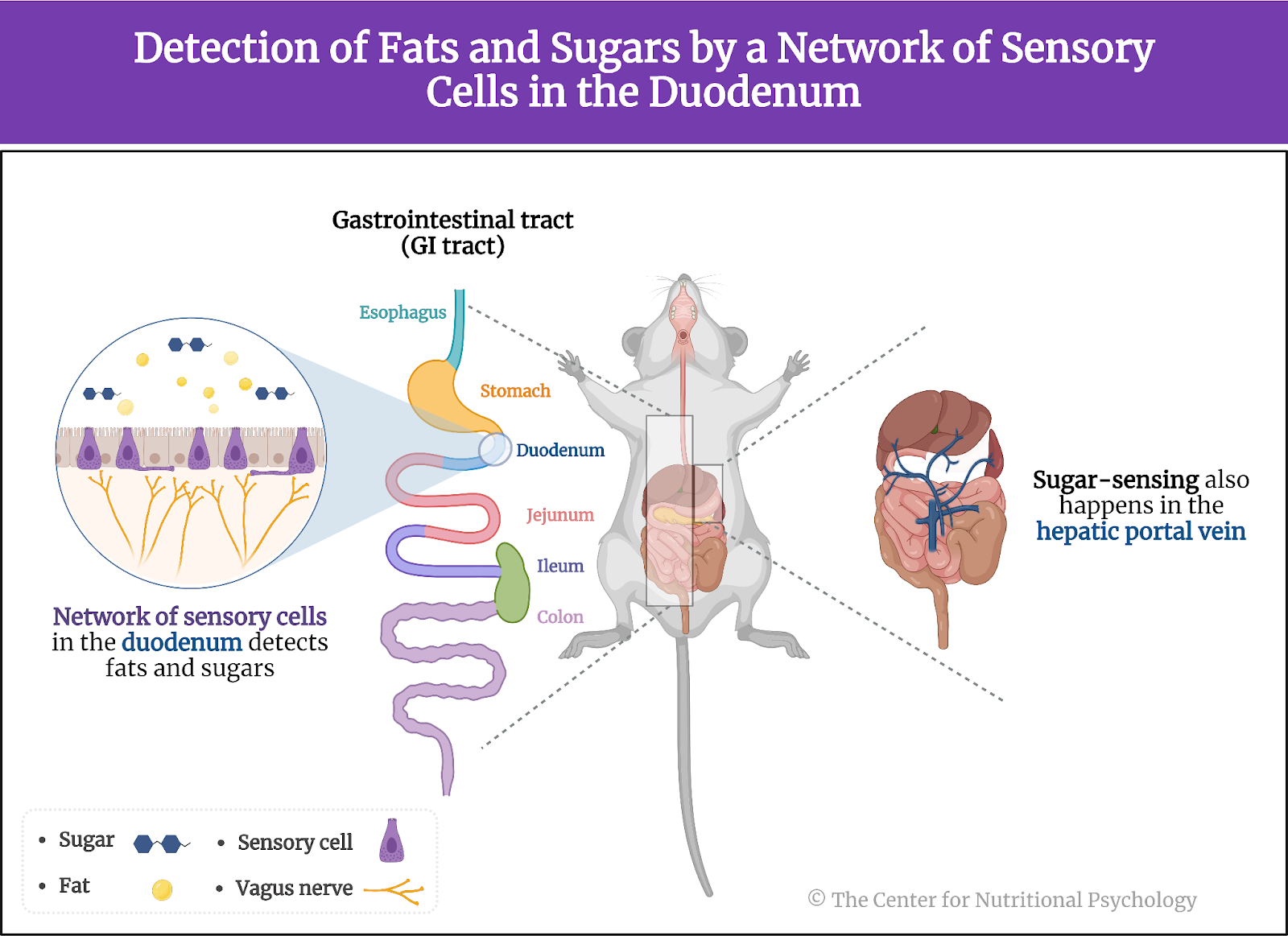
Figure 5. Detection of fats and sugars by a network of sensory cells in the duodenum
Reinforcement learning based on sugar and fat happens through separate circuits
Experiments where researchers destroyed fat-sensing neurons but left the sugar-sensing ones intact or vice versa indicated that reinforcement learning, a type of learning where a mouse can associate a specific object or sensation with a specific nutrient, can be conducted using only the neurons sensing that specific nutrient. Mice without fat-sensing neurons but with intact sugar-sensing neurons were able to form a preference for a flavor associated with sugar intake.
Mice without fat-sensing neurons but with intact sugar-sensing neurons were able to form a preference for a flavor associated with sugar intake
In the nigrostriatal region of the brain, both information about fat and sugar in the gut led to the release of dopamine (thought to produce the feeling of pleasure and a rewarding experience). However, these nutrients activated parallel and largely separate neuronal populations at each node of the reward circuit in this part of the brain. This means that distinguishable neural circuits are responsible for reinforcement learning for fat and sugar, i.e., for learning to associate stimuli with pleasure caused by the ingestion of sugar and pleasure caused by the ingestion of fat (see Figure 6).

Figure 6. Release of dopamine in response to fat and sugar
Consuming fat and sugar at the same time promotes overeating for pleasure
In another group of experiments, study authors found that when they gave mice a choice between taking solutions of fat, sugar (sucrose), or a mixture of the two nutrients, mice consumed equal amounts of fat or sugar solutions. However, the number of licks of the solution containing both sugar and fats nearly doubled compared to just sugar or just fat alone.
Consuming fat and sugar at the same time promotes overeating for pleasure
Researchers then offered mice a non-nutrient-flavored solution to lick, injecting sugar, fat, or a combination of the two directly into their guts (using the catheters they installed). After training to pair a non-nutritive flavor with a solution, mice again showed a preference for the mixed solution (both sugar and fat), indicating that the preference for this solution is independent of taste. This means that the preference for the sugar and fat combination has to do with sensing those nutrients in the gut and not with their taste in the mouth.
The preference for the sugar and fat combination has to do with sensing those nutrients in the gut and not with their taste in the mouth
Study authors conclude that this is because this mixed solution activates both the brain’s rewarding circuits for fat and sugar, increasing the overall feeling of pleasure. Analysis of the quantity of released dopamine in the dorsal striatum region of the brain found that it is much higher after the injection of the mixed sugar-fat solution than after the injection of a solution with equal caloric value but containing only fat.
This suggests that foods rich in fat and sugar produce higher activation of reward circuits for the same amount of calories than foods containing just one of these two nutrients. This would translate to higher feelings of pleasure after consumption, motivating the individual to consume more food of that type, which could lead to obesity (see Figure 7).
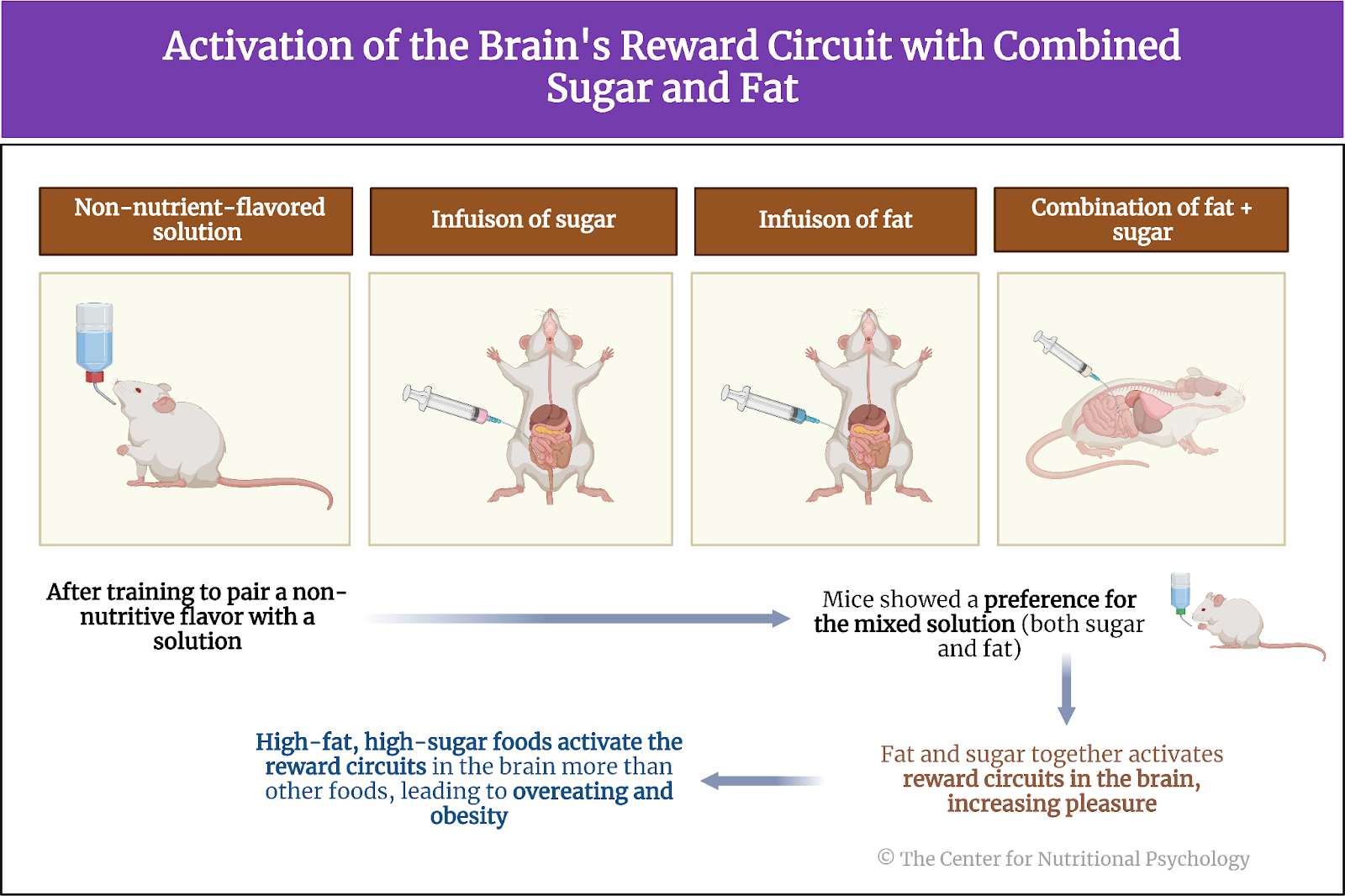
Figure 7. Activation of the brain’s rewarding circuits with combined sugar and fat
Conclusion
The study showed that sensing the presence of sugars and fats in the intestines of mice is achieved through different sets of neurons. The study also found that these two types of nutrients activate parallel but largely separate reward circuits in the brain. Due to this, consuming foods that contain both sugars and fats activates reward circuits in the brain for both of these substances, resulting in a higher release of dopamine and, thus, higher feelings of pleasure, compared to consuming foods of equal caloric value but containing only fats or only sugars. These peculiarities of neural pathways make mice, and possibly humans, more likely to overeat foods rich in fats and sugars driven by feelings of pleasure the simultaneous activation of these two neural pathways creates.
The discovery of these separate mechanisms and understanding of the ways they work can help scientists. Still, people working in nutrition better understand how the properties of certain food items lead to obesity. This can, in sequence, help better plan individual diets and develop policies to help stop the ongoing obesity epidemic.
The paper “Separate gut-brain circuits for fat and sugar reinforcement combine to promote overeating” was authored by Molly McDougle, Alan de Araujo, Arashdeep Singh, Mingxin Yang, Isadora Braga, Vincent Paille, Rebeca Mendez-Hernandez, Macarena Vergara, Lauren N. Woodie, Abhishek Gour, Abhisheak Sharma, Nikhil Urs, Brandon Warren, and Guillaume de Lartigue.
References
Bonaz, B., Bazin, T., & Pellissier, S. (2018). The vagus nerve at the interface of the microbiota-gut-brain axis. In Frontiers in Neuroscience (Vol. 12, Issue FEB). Frontiers Media S.A. https://doi.org/10.3389/fnins.2018.00049
Hedrih, V. (2023). Scientists Propose that Ultra-Processed Foods be Classified as Addictive Substances. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/scientists-propose-that-ultra-processed-foods-be-classified-as-addictive-substances/
Ikemoto, S., Takahashi, M., Tsunoda, N., Maruyama, K., Itakura, H., & Ezaki, O. (1996). High-fat diet-induced hyperglycemia and obesity in mice: Differential effects of dietary oils. Metabolism, 45(12), 1539–1546. https://doi.org/10.1016/S0026-0495(96)90185-7
McDougle, M., de Araujo, A., Singh, A., Yang, M., Braga, I., Paille, V., Mendez-Hernandez, R., Vergara, M., Woodie, L. N., Gour, A., Sharma, A., Urs, N., Warren, B., & de Lartigue, G. (2024). Separate gut-brain circuits for fat and sugar reinforcement combine to promote overeating. Cell Metabolism. https://doi.org/10.1016/j.cmet.2023.12.014
Pujol, J., Blanco-Hinojo, L., Martínez-Vilavella, G., Deus, J., Pérez-Sola, V., & Sunyer, J. (2021). Dysfunctional Brain Reward System in Child Obesity. Cerebral Cortex, 31, 4376–4385. https://doi.org/10.1093/cercor/bhab092
Seabrook, L. T., Naef, L., Baimel, C., Judge, A. K., Kenney, T., Ellis, M., Tayyab, T., Armstrong, M., Qiao, M., Floresco, S. B., & Borgland, S. L. (2023). Disinhibition of the orbitofrontal cortex biases decision-making in obesity. Nature Neuroscience, 26(1), 92–106. https://doi.org/10.1038/s41593-022-01210-6
Wilding, J. P. H. (2001). Causes of obesity. Practical Diabetes International, 18(8), 288–292. https://doi.org/10.1002/PDI.277
Wong, M. C., Mccarthy, C., Fearnbach, N., Yang, S., Shepherd, J., & Heymsfield, S. B. (2022). Emergence of the obesity epidemic: 6-decade visualization with humanoid avatars. The American Journal of Clinical Nutrition, 115(4), 1189–1193. https://doi.org/10.1093/AJCN/NQAC005





Leave a comment