- An analysis of UK Biobank data published in Nature Communications showed that individuals adhering to the EAT-Lancet diet have a lower risk of depression and anxiety.
- The group with the highest adherence to this diet had around 20% lower risk of depression and anxiety compared to the lowest adherence group.
- The EAT-Lancet diet emphasizes plant-based foods, moderate animal product consumption, and limited processed and red meat intake.
We can often read that eating certain foods might be good for our health. Studies frequently report that heightened or decreased intake of a certain type of food is associated with increased or reduced risk of certain diseases. For example, regular consumption of refined sugars, particularly sugary drinks, has been linked to a host of adverse health outcomes (Hedrih, 2023; Huang et al., 2023). On the other hand, snacking on whole almonds has been found to reduce LDL cholesterol and improve endothelial function (Dikariyanto et al., 2020) and was, therefore, beneficial for overall health.
These findings refer to individual foods or food components. However, scientists also study the effects of broad dietary patterns on health and overall well-being.
Regular consumption of refined sugars has been linked to a host of adverse health outcomes.
Dietary patterns
A dietary pattern is the overall composition and combination of foods and beverages one consumes over time. It’s not just about individual nutrients but the synergistic effects of various foods in a person’s diet. Examples of dietary patterns include the Mediterranean diet, which emphasizes whole grains, vegetables, and healthy fats, and the MIND diet, which focuses on brain health. These patterns define an individual’s long-term eating habits. Scientists have defined certain broad dietary patterns that individuals’ diets can be compared to for research purposes. These diets reflect the general dietary habits of certain groups and cultures or are created by scientists to improve health or research a certain topic.
For example, many studies explore the associations between the Western diet and health, finding that adherence to this diet is linked to various adverse health outcomes. The Western diet is characterized by a high intake of processed foods, red and processed meats, refined grains, sugars, and unhealthy fats (Hayes et al., 2024). On the other hand, studies link adherence to the Mediterranean diet and the Nordic diet with beneficial health outcomes (Adamsson et al., 2012; Araste et al., 2024; Camprodon-Boadas et al., 2024; Poulsen et al., 2014; The InterAct Consortium, 2011).
A dietary pattern is the overall combination and frequency of foods and beverages a person consumes regularly.
The EAT-Lancet diet
In January 2019, the EAT-Lancet Commission, a group of scientists and experts, developed recommendations for a sustainable and healthy diet that can support human health and environmental stability. The Commission based its diet on the best available evidence for what constitutes a healthy diet and considered food production sustainability. Their recommendations were published in the Lancet, one of the leading scientific journals in the world (Willett et al., 2019).
The EAT-Lancet diet is largely plant-based. It consists of whole grains, fruits, vegetables, nuts, legumes, unsaturated oils, low to moderate amounts of seafood and poultry, and no or low red meat, processed meat, added sugar, refined grains, and starchy vegetables. Adherence to this diet would represent a substantial dietary shift for most people. Adopting worldwide would require the global consumption of healthy foods to double, halving the consumption of less nutritious foods (Dalile et al., 2022).
The current study
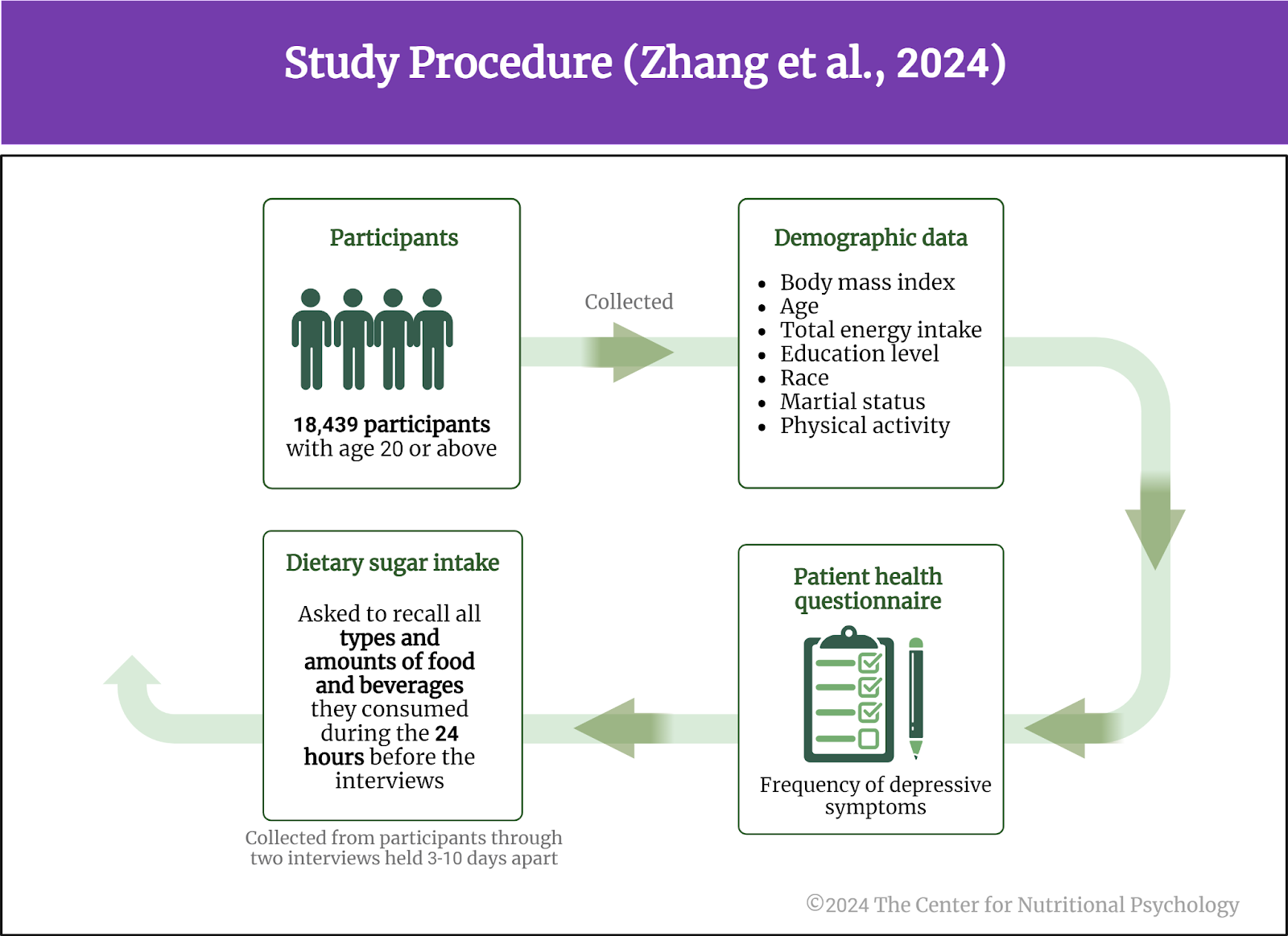
Study author Xujia Lu and her colleagues wanted to explore how adherence to the EAT-Lancet diet might be associated with anxiety and depression among UK adults (Lu et al., 2024). They analyzed data from the UK Biobank, a large-scale biomedical database and research resource containing health and genetic information from half a million U.K. participants. This database is available for scientific purposes to researchers worldwide.
This study used data from 180,466 participants. At the start of the study, their average age was 56 years, and 46% were male.
These participants completed a dietary questionnaire called Oxford WebQ. This questionnaire asks participants to recall their food and drink intake in the previous 24 hours. Some participants completed it when they were included in the UK Biobank group, and all participants received invitations to complete it on multiple occasions.
Study authors used these data to calculate how much participants’ diets resembled the EAT-Lancet diet (i.e., how much participants adhered to it). There is currently no consensus about the right way to calculate adherence to the EAT-Lancet diet, so the study authors created several different scores to express this adherence. Data about depression and anxiety came from participants’ reports, hospital data, and the death registry records.
Individuals adhering to the EAT-Lancet diet were less likely to suffer from depression and anxiety
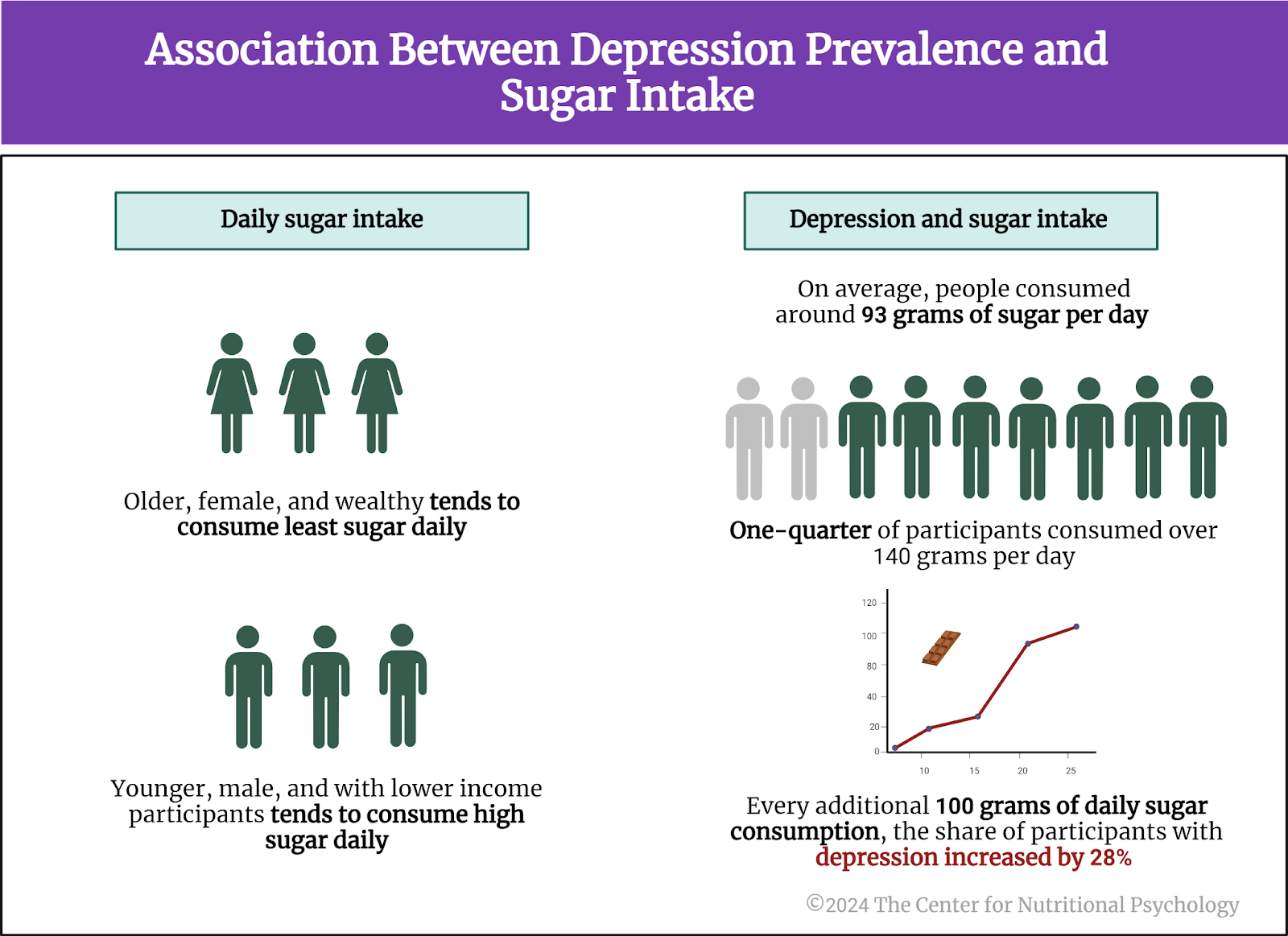
During the follow-up of around 11-12 years on average, 4548 cases of depression, 6026 cases of anxiety, and 1262 individuals with both depression and anxiety were identified.
Depending on the way adherence to the EAT-Lancet diet was calculated, participants with the strongest adherence to the EAT-Lancet diet had between 16% and 26% lower risk of developing depression or anxiety disorders compared to those with the lowest adherence to the EAT-Lancet diet. The risk reduction was the strongest for the co-occurrence of depression and anxiety, i.e., for suffering from both depression and anxiety at the same time (see Figure 1).

Figure 1. Study procedure and findings (Lu et al., 2024)
Participants with the strongest adherence to the EAT-Lancet diet had between 16% and 26% lower risk of developing depression or anxiety disorders.
Participants with higher adherence to the EAT-Lancet diet were more likely to be women, slightly older, nonsmokers, more physically active, and have lower body mass index and total energy intake.
Conclusion
Overall, the study suggests that higher adherence to the EAT-Lancet diet is associated with lower risks of depression, anxiety, and co-occurrence. Individuals adhering to this diet also tended to have healthier lifestyle habits.
The design of this study does not allow any cause-and-effect conclusions to be derived from the results. Because of this, we do not know whether this dietary pattern itself reduces the risk of anxiety and depression. It is also possible that factors producing the lowered risk of depression and anxiety make individuals more likely to adhere to a healthy diet. Still, it is possible that promoting the dietary pattern described by the EAT-Lancet diet might help prevent depression and anxiety.
The paper “Adherence to the EAT-Lancet diet and incident depression and anxiety” was authored by Xujia Lu, Luying Wu, Liping Shao, Yulong Fan, Yalong Pei, Xinmei Lu, Yan Borné, and Chaofu Ke.
References
Adamsson, V., Reumark, A., Cederholm, T., Vessby, B., Risérus, U., & Johansson, G. (2012). What is a healthy Nordic diet? Foods and nutrients in the NORDIET study. Food & Nutrition Research, 56(1), 18189. https://doi.org/10.3402/fnr.v56i0.18189
Araste, A., Moghadam, M. R. S. F., Mohammadhasani, K., Fard, M. V., Khorasanchi, Z., Latifi, M., Hasanzadeh, E., Talkhi, N., Sharifan, P., Asadiyan-Sohan, P., Bidokhti, M. K., Ghassemi, A., Darban, R. A., Ferns, G., & Ghayour-Mobarhan, M. (2024). Adherence to the Nordic diet is associated with anxiety, stress, and depression in recovered COVID-19 patients, a case-control study. BMC Nutrition, 10(1), 38. https://doi.org/10.1186/s40795-024-00845-x
Camprodon-Boadas, P., Gil-Dominguez, A., De La Serna, E., Sugranyes, G., Lázaro, I., & Baeza, I. (2024). Mediterranean Diet and Mental Health in Children and Adolescents: A Systematic Review. Nutrition Reviews, nuae053. https://doi.org/10.1093/nutrit/nuae053
Dalile, B., Kim, C., Challinor, A., Geurts, L., Gibney, E. R., Galdos, M. V., Fata, G. L., Layé, S., Mathers, J. C., Vauzour, D., Verkuyl, J. M., & Thuret, S. (2022). The EAT–Lancet references diet and cognitive function across the life course. The Lancet Planetary Health, 6(9), e749–e759. https://doi.org/10.1016/S2542-5196(22)00123-1
Dikariyanto, V., Smith, L., Francis, L., Robertson, M., Kusaslan, E., O’Callaghan-Latham, M., Palanche, C., D’Annibale, M., Christodoulou, D., Basty, N., Whitcher, B., Shuaib, H., Charles-Edwards, G., Chowienczyk, P. J., Ellis, P. R., Berry, S. E. E., & Hall, W. L. (2020). Snacking on whole almonds for 6 weeks improves endothelial function and lowers LDL cholesterol but does not affect liver fat and other cardiometabolic risk factors in healthy adults: The ATTIS study, a randomized controlled trial. The American Journal of Clinical Nutrition, 111(6), 1178–1189. https://doi.org/10.1093/AJCN/NQAA100
Hayes, A. M. R., Lauer, L. T., Kao, A. E., Sun, S., Klug, M. E., Tsan, L., Rea, J. J., Subramanian, K. S., Gu, C., Tanios, N., Ahuja, A., Donohue, K. N., Décarie-Spain, L., Fodor, A. A., & Kanoski, S. E. (2024). Western diet consumption impairs memory function via dysregulated hippocampus acetylcholine signaling. Brain, Behavior, and Immunity, 118, 408–422. https://doi.org/10.1016/j.bbi.2024.03.015
Hedrih, V. (2023, June 6). Health Consequences of High Sugar Consumption. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/health-consequences-of-high-sugar-consumption/
Huang, Y., Chen, Z., Chen, B., Li, J., Yuan, X., Li, J., Wang, W., Dai, T., Chen, H., Wang, Y., Wang, R., Wang, P., Guo, J., Dong, Q., Liu, C., Wei, Q., Cao, D., & Liu, L. (2023). Dietary sugar consumption and health: Umbrella review. BMJ (Clinical Research Ed.), 381, e071609. https://doi.org/10.1136/bmj-2022-071609
Lu, X., Wu, L., Shao, L., Fan, Y., Pei, Y., Lu, X., Borné, Y., & Ke, C. (2024). Adherence to the EAT-Lancet diet and incident depression and anxiety. Nature Communications, 15(1), 5599. https://doi.org/10.1038/s41467-024-49653-8
Poulsen, S. K., Due, A., Jordy, A. B., Kiens, B., Stark, K. D., Stender, S., Holst, C., Astrup, A., & Larsen, T. M. (2014). Health effect of the New Nordic Diet in adults with increased waist circumference: A 6-mo randomized controlled trial1234. The American Journal of Clinical Nutrition, 99(1), 35–45. https://doi.org/10.3945/ajcn.113.069393
The InterAct Consortium. (2011). Mediterranean Diet and Type 2 Diabetes Risk in the European Prospective Investigation Into Cancer and Nutrition (EPIC) Study. Diabetes Care, 34(9), 1913–1918. https://doi.org/10.2337/dc11-0891
Willett, W., Rockström, J., Loken, B., Springmann, M., Lang, T., Vermeulen, S., Garnett, T., Tilman, D., DeClerck, F., Wood, A., Jonell, M., Clark, M., Gordon, L. J., Fanzo, J., Hawkes, C., Zurayk, R., Rivera, J. A., Vries, W. D., Sibanda, L. M., … Murray, C. J. L. (2019). Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. The Lancet, 393(10170), 447–492. https://doi.org/10.1016/S0140-6736(18)31788-4