Within nutritional psychology, we explore the dietary and nutritional elements influencing the diet-mental health relationship. This involves identifying the processes and mechanisms through which our diet and dietary intake patterns influence our brain, behavior, and experience. Sugar intake is a substantial and increasing part of the human diet. Understanding its influence on our diet-mental health relationship is important within nutritional psychology. Let’s look at a recent study published in the BMJ that explores the sugar-health connection.
This umbrella review by Huang and colleagues (2023) reviewed 73 meta-analytic articles exploring the connection between sugar consumption and adverse health outcomes. In this study, findings reported that sugar consumption is associated with many adverse health outcomes. Specifically, this study identified associations between sugar consumption and eighteen harmful metabolic issues, ten harmful cardiovascular conditions, seven types of cancer, and ten other types of adverse medical conditions. The best quality evidence was for links between sugar consumption and increased body weight (Huang et al., 2023).
Studies have shown an association between sugar consumption and certain metabolic and cardiovascular issues, cancer, obesity, and other adverse medical conditions.
Sugars and carbohydrates
Carbohydrates are a type of molecule that provides the body with energy. Alongside protein and fat, carbohydrates are considered macronutrients, nutrients the human body requires in large quantities. The three main types of carbohydrates are sugars, starches, and fibers (Slavin, 2013) (see Figure 1).
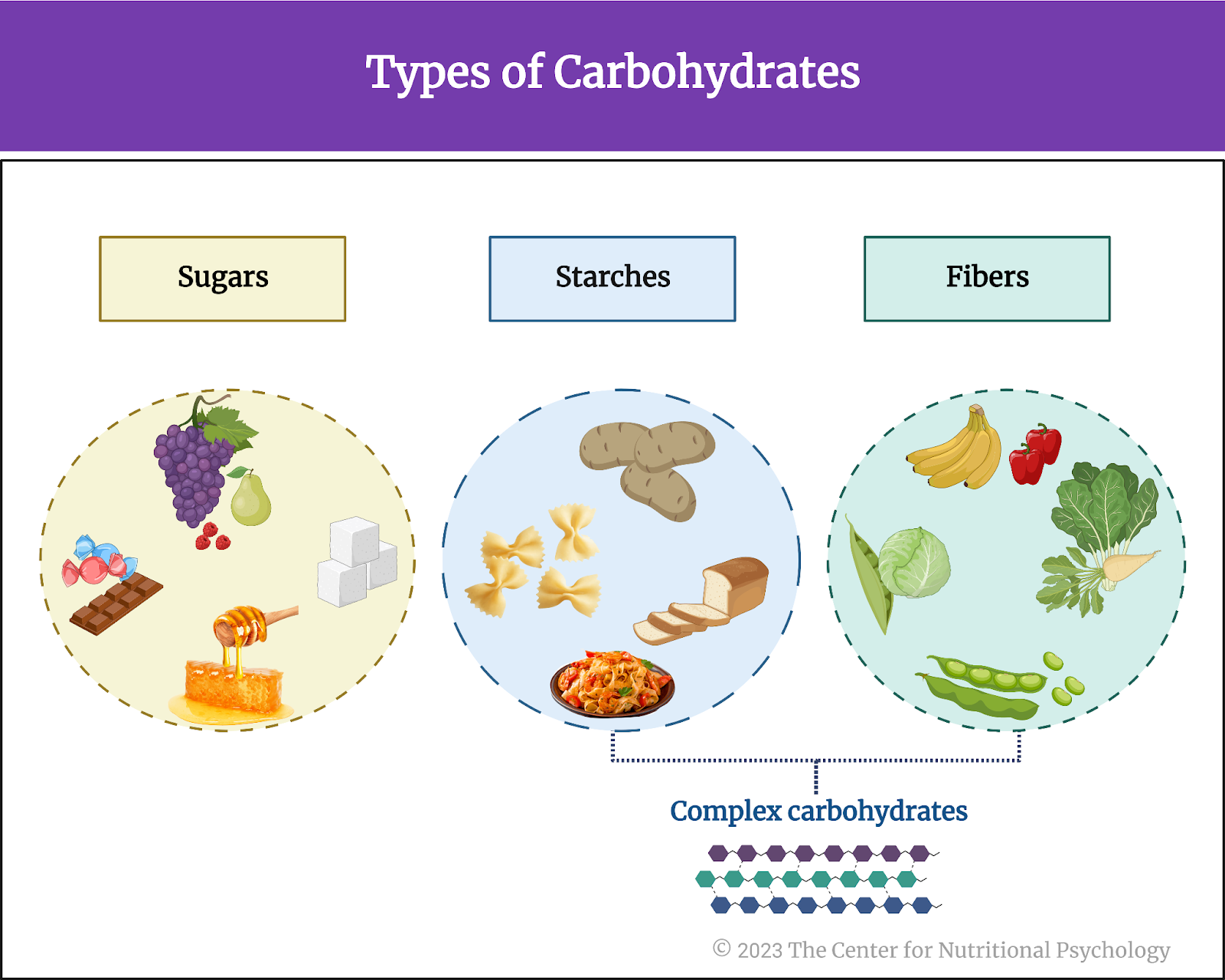
Figure 1. Three types of carbohydrates
Fibers and starches are called complex carbohydrates, made of many simple carbohydrates strung together to form large molecules. They need to be broken down by the body into simple carbohydrates to be used. The human body can break down and digest starches, such as those found in bread, cereals, or pasta, but it cannot digest most fibers. However, eating foods containing fiber can help an individual feel full (satiated) and be less likely to overeat (Cho et al., 2010; Samra & Anderson, 2007).
Eating foods containing fiber can help one feel satiated and be less likely to overeat.
Sugars
Sugars are called simple carbohydrates because their molecules are the smallest and the simplest. The three most common sugars are glucose (the primary source of energy for the cells of our body), fructose (the naturally occurring sugar found in fruits, honey, and vegetables), and sucrose (the substance sold in supermarkets as “sugar,” a combination of glucose and fructose, also naturally occurring).
Sugars are naturally found in various fruits, vegetables, and animal products (e.g., honey, milk, meat). However, sugars are also very often added to food and drinks, either by the cook or the manufacturer, during food production and preparation, or directly by the consumer, before consumption. This is done to increase the sweetness of food, thus making it tastier. Researchers refer to sugars added to food and beverages in this way as “added sugars” (Huang et al., 2023).
Added sugars
Generally, sugar-sweetened beverages are the largest source of added sugars. These include soft drinks (both carbonated and non-carbonated), fruit drinks, and sports and energy drinks. Milkshakes, smoothies, and similar sweetened drinks also contain added sugar.
Foods with lots of added sugar include various desserts, candies, cakes, sweet snacks, ice cream, granola and energy bars, milk chocolate, candied dried fruits, canned fruits, sweetened flavored yogurts, many condiments (such as ketchup), most cereals, cocoa spreads, creamers, jams, and many others (see Figure 2).

Figure 2. Foods containing lots of added sugars
What are the health consequences of high sugar consumption?
Although the Dietary Guidelines for Americans by the United States Department of Agriculture recommend that between 45% and 65% of calories in our diet should come from carbohydrates, they also suggest that the intake of added sugars should be very limited or altogether avoided. Sources such as the Harvard T.H. Chan School of Public Health website specify that the body needs no carbohydrates from added sugar. Despite this, foods and drinks with added sugars represent a large share of people’s dietary intake worldwide, with consumption increasing in many developing countries. This is particularly true with sugar-sweetened beverages such as soft drinks (Huang et al., 2023).
The body does not need carbohydrates from added sugar. Yet, foods and drinks with added sugars represent a large share of the dietary intake of people worldwide.
Numerous studies have linked a high intake of sugars with an increased risk of various adverse health outcomes. These include obesity, diabetes, cardiovascular disease, dental caries, and abnormal fat accumulation in tissues where fat is not normally stored, such as the liver, muscles, pancreas, heart, and others.
The current study
Study author Yin Huang from the Sichuan University in Chengdu, China, and his colleagues wanted to evaluate the quality of evidence, potential biases, and validity of all available studies on dietary sugar consumption and health outcomes.
The number of scientific studies exploring links between the consumption of sugars and health runs in hundreds of thousands worldwide, and new ones are conducted and published daily. These researchers conducted an umbrella review.
The number of scientific studies exploring links between the consumption of sugars and health runs in hundreds of thousands worldwide.
What is an umbrella review?
When a certain topic attracts a lot of research interest, many studies are conducted to explore that topic further. Studies are conducted by different researchers. They use more or less different methodologies and can also conceptualize key factors they explore in ways that are not completely identical.
Scientists need ways to integrate the multitudes of findings produced in this way. To do this, they can conduct systematic reviews, evaluating the findings of different studies and discussing similarities and differences between their methodologies and findings. When there are many studies (e.g., more than a dozen) that explore the same link between certain factors or the same aspect of some phenomenon, a meta-analysis can be conducted to map the strength of the links observed and make quantitative inferences about tendencies in the findings of these studies.
Finally, when the number of studies on a topic is really large, and their study methodologies and factors are diverse (i.e., there are many systematic reviews and meta-analyses), the type of study that can integrate their results is called the umbrella review. An umbrella review is a type of systematic review that combines evidence from a multitude of systematic reviews and meta-analyses on a certain topic (see Figure 3).
It starts with a rigorous process of searching and selecting relevant systematic reviews and meta-analyses to include in the study. Assessing the quality of the included studies and integrating the findings of different reviews follows. Its very name indicates a study incorporating the results of many integrating studies (see Figure 3).

Figure 3. Set-up of an umbrella review
The procedure
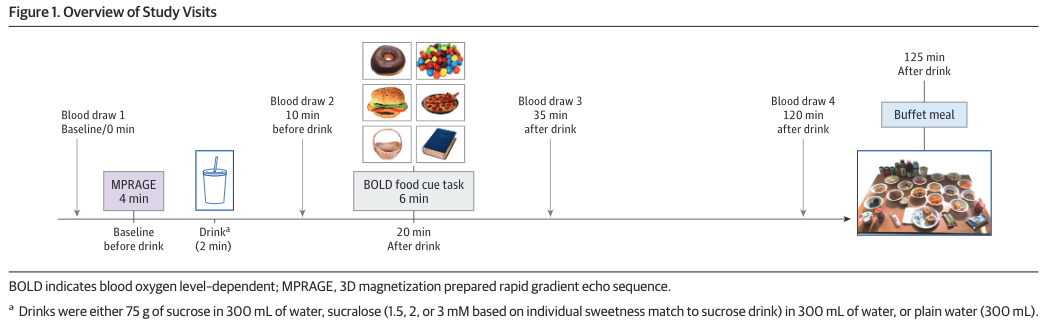
The authors searched publicly available databases of research publications for systematic reviews and meta-analyses that studied the health outcomes of sugar consumption. They considered studies of sugar consumption that measured the specific proportion of sugars in foods, the percentage of total energy derived from sugars, or combinations of these two. They searched PubMed, Embase, Web of Science, and the Cochrane Database of Systematic Reviews from inception through January 2022. They looked for papers written in English.
They used “sugars” or “sugar” and “systematic review” or “meta-analysis” as keywords for their searches. Two of the authors conducted the searches separately. A third author resolved any discrepancies between their literature screening results.
Search results
The search yielded 8601 research papers—2184 of those turned out to be duplicates and were excluded. Of the remaining 6417 papers, 6221 were excluded from further analysis for various reasons. This left 196 papers with eligible titles and abstracts. Of these, researchers excluded a further 124 because data on sugar could not be extracted from them, because they were reviewed without meta-analyses, or due to various methodological issues. 4 turned out not to be in English and were thus excluded.
In the end, 73 scientific articles contained results of meta-analyses and met all the inclusion criteria set by the researchers. These papers were included in the umbrella analysis.
The quality of evidence
An important aspect these researchers considered when analyzing was the quality of evidence presented for the claims made in the analyzed papers. Not all scientific findings are the same. Some findings are obtained on large samples that are likely to be representative of studied populations. They describe strong and clear effects of one studied factor on another or strong associations between phenomena. Such studies are considered to provide strong evidence. When the physical mechanism creating the claimed effects is known, or at least when researchers have a plausible idea of what it might be, the evidence is even stronger.
However, studies are sometimes done on small samples that are or might be quite different from the population. They might report associations between studied phenomena without any further knowledge or idea about the physical mechanism creating the reported link. And the links reported might be very weak, sometimes so weak that one might suspect they are simply due to chance. The evidence quality provided by such studies is considered to be much worse.
In the case of this study, researchers classified meta-analytic studies they analyzed into five categories based on the strength of the evidence. The highest evidence strength was assigned to studies conducted on very large samples (over 1000 cases or over 20,000 participants, depending on the features of the studied phenomena) and reported strong effects or associations similar across different studies covered by the meta-analysis analyzed. On the other hand, studies that reported results that were near zero or were very weak were considered to provide weak evidence for the associations reported. Sample sizes were taken into account because it is much, much easier to obtain small samples that are unusual and thus provide unusual results than large samples (Hedrih & Hedrih, 2022).
They assigned these evidence classes numbers ranging from 1 (best quality evidence) to 4 (weakest evidence) and N.S. (no association at all, N.S. stands for non-significance).
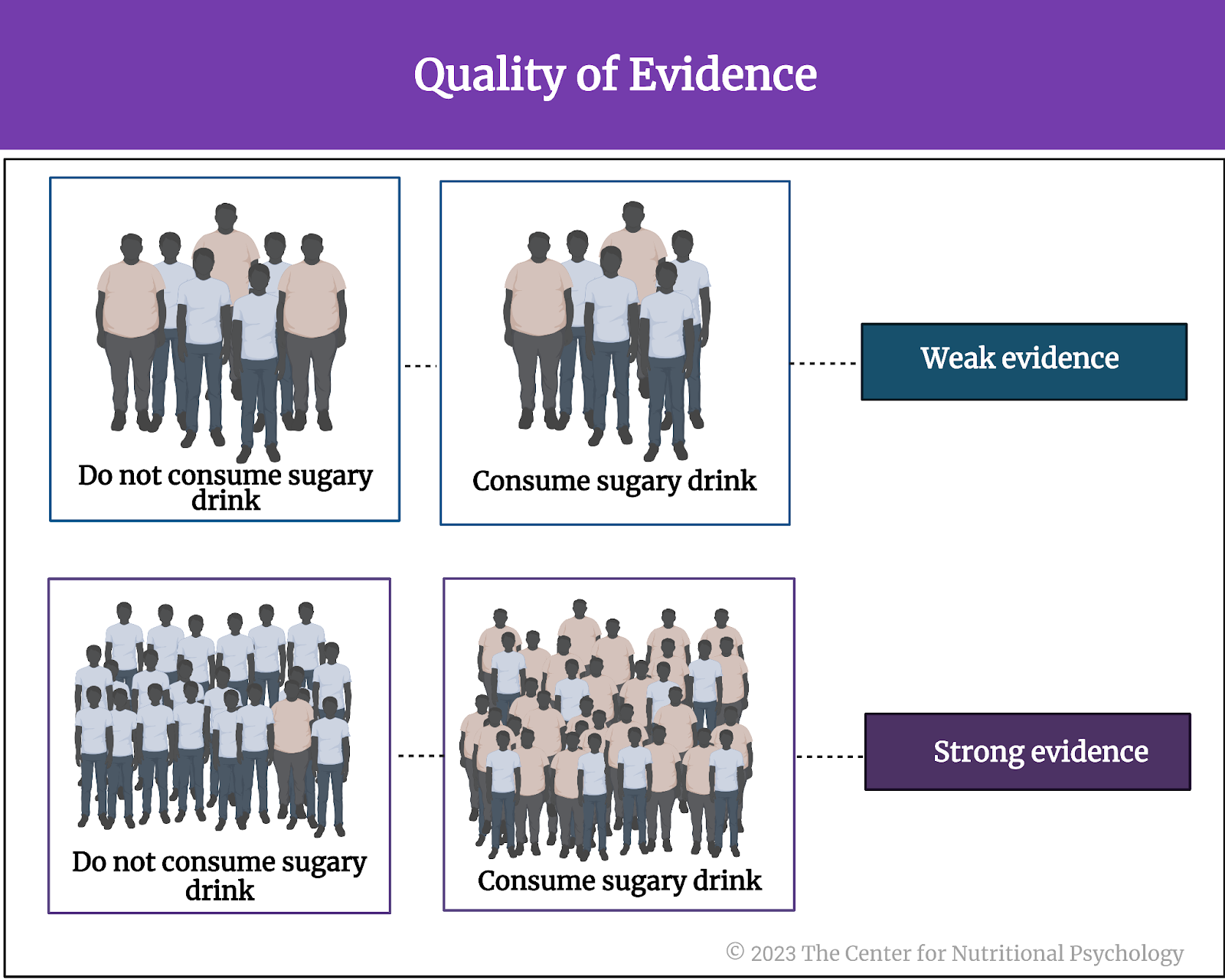
Figure 4. Quality of evidence
High sugar consumption is associated with four beneficial and 45 harmful health outcomes.
Results showed that most of the meta-analyses included in the study studied associations between the consumption of sugar and endocrine/metabolic diseases (such as diabetes, 28 such studies), cancer (25 studies), and cardiovascular diseases (17) (see Figure 5).
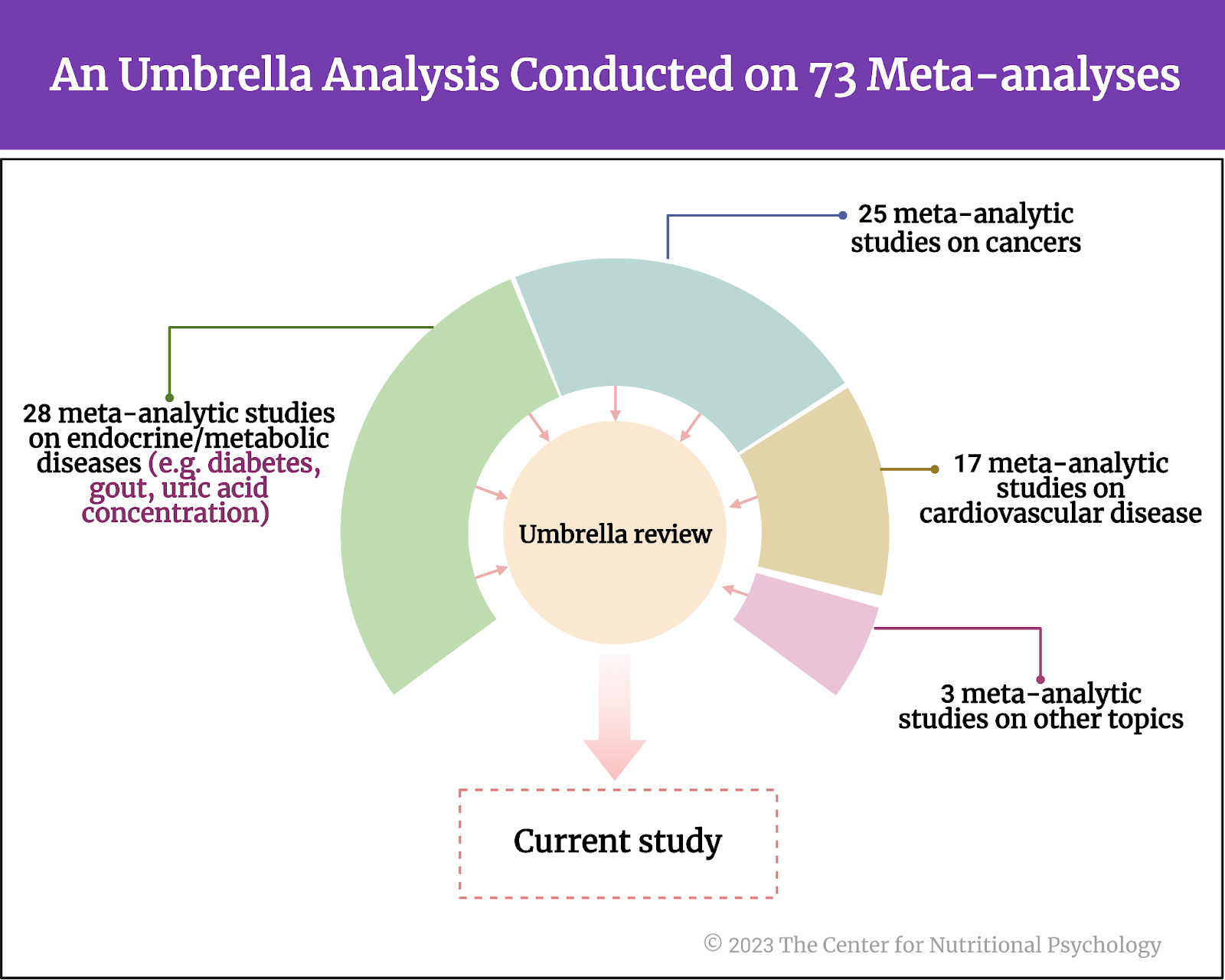
Figure 5. The contents of this umbrella review
These studies reported four beneficial associations between high sugar consumption and medical outcomes and 45 harmful ones. Thirty-four studies reported no associations between sugar consumption and the health outcomes they examined.
Children who consume more sweetened beverages have a 55% higher chance of being obese.
Higher consumption of sugar-sweetened beverages was associated with higher body weight and a higher risk of gout (class 4 evidence). Gout is arthritis characterized by a buildup of uric acid crystals in the joints that cause inflammation and pain.
Children who consumed high quantities of sugar-sweetened beverages had a 55% higher likelihood of being obese compared to children who did not consume such beverages (class 2 evidence). The more frequently children consumed such beverages, the higher their body mass was.
Children who consumed high quantities of sugar-sweetened beverages had a 55% higher likelihood of being obese than children who did not.
Sugar consumption, coronary heart disease, and cancer
One study linked a higher intake of sugar-sweetened beverages with the risk of coronary heart disease. They reported that every additional glass of sugar-sweetened beverages (250 mL) per day was associated with a 17% increase in the risk of coronary heart disease (class 2 evidence). Another study linked higher consumption of these beverages with an increased likelihood of myocardial infarction (class 3 evidence).
Every additional glass of sugar-sweetened beverages (250 mL) per day was associated with a 17% increase in the risk of coronary heart disease.
One meta-analysis reported that participants who consumed sugar-sweetened beverages the most had a two times higher risk of developing hepatocellular carcinoma (a type of liver cancer, class 4 evidence). Another meta-analysis linked higher fructose intake with a higher risk of pancreatic cancer (class 3 evidence).
Other health outcomes
A recent meta-analysis reported that every additional glass (250 mL) of sugar-sweetened beverages per day was associated with a 4% increase in death from all causes (class 3 evidence). Another study reported a link between higher consumption of these drinks and depression (class 2 evidence).
Researchers also reported several other health outcomes linked to sugar consumption, but the evidence for those associations was very weak (class 4). These included links between increased consumption of sugar-sweetened beverages and hypertension, death from cardiovascular disease, prostate cancer, death from breast cancer, overall risk of death from cancer, risk of asthma, fatty liver disease, bone mineral density, and others.
Health outcomes not associated with sugar include the risk of colorectal cancer, ovarian cancer, and death from cardiovascular disease. Fructose intake was not associated with type 2 diabetes, risk of hypertension, and uric acid concentrations in the serum. Consumption of sugar of sugar-sweetened beverages was not found to be associated with the risk of chronic kidney disease. Do remember that all the studies conducted are meta-analyses.
Conclusion
The analysis showed that high dietary sugar intake is associated with various harmful health outcomes. Although evidence was strongest for the effects of high intake of sugars on increased body weight, particularly in children, the evidence for other adverse health effects is also considerable. These findings come from a series of meta-analyses, each of which integrated findings of multitudes of individual studies conducted in different places and on different people worldwide, giving extra weight to the reported results.
The insights from these studies can help better educate the general population about health outcomes related to nutritional choices, particularly consuming food and beverages with extreme quantities of added sugars. They can also be useful to manufacturers of food and beverages as a guide to make future food products healthier.
The paper “Dietary sugar consumption and health: umbrella review” was authored by Yin Huang, Zeyu Chen, Bo Chen, Jinze Li, Xiang Yuan, Jin Li, Wen Wang, Tingting Dai, Hongying Chen, Yan Wang, Ruyi Wang, Puze Wang, Jianbing Guo, Qiang Dong, Chengfei Liu, Qiang Wei, Dehong Cao, and Liangren Liu.
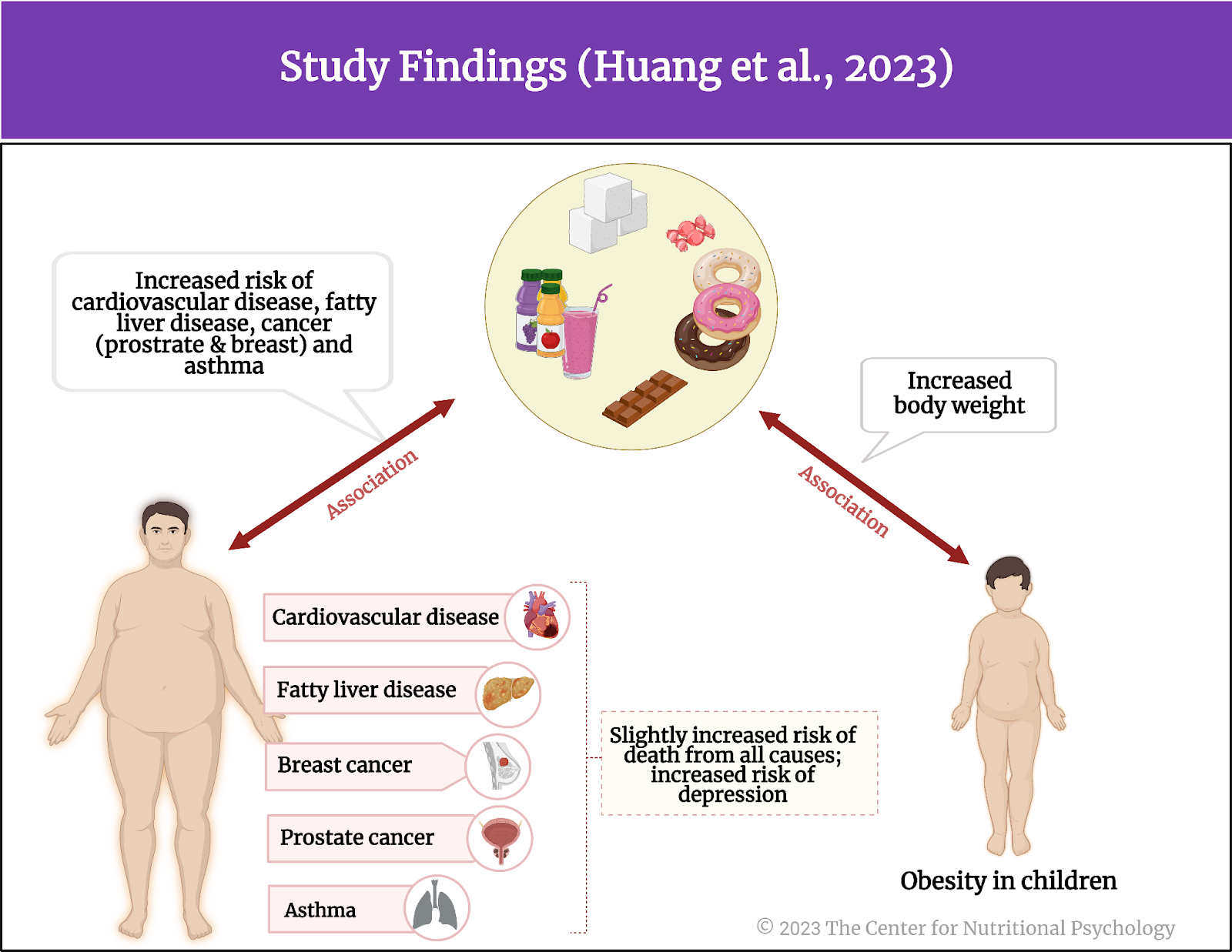
Figure 6. Study findings of the umbrella review
References
Cho, S., Case, I., & Nishi, S. (2010). Fiber and Satiety. In Weight Control and Slimming Ingredients in Food Technology (pp. 227–276). Blackwell Publishing Ltd.
Hedrih, V., & Hedrih, A. (2022). Interpreting statistics for beginners : a guide for behavioural and social scientists. Routledge, Taylor&Francis Group. https://doi.org/10.4324/9781003107712
Huang, Y., Chen, Z., Chen, B., Li, J., Yuan, X., Li, J., Wang, W., Dai, T., Chen, H., Wang, Y., Wang, R., Wang, P., Guo, J., Dong, Q., Liu, C., Wei, Q., Cao, D., & Liu, L. (2023). Dietary sugar consumption and health: umbrella review. BMJ (Clinical Research Ed.), 381, e071609. https://doi.org/10.1136/bmj-2022-071609
Samra, R. A., & Anderson, G. H. (2007). Insoluble cereal fiber reduces appetite and short-term food intake and glycemic response to food consumed 75 min later by healthy men. The American Journal of Clinical Nutrition, 86(4), 972–979. https://doi.org/10.1093/AJCN/86.4.972
Slavin, J. L. (2013). Carbohydrates, dietary fiber, and resistant starch in white vegetables: Links to health outcomes. Advances in Nutrition, 4(3), 3515–3555. https://doi.org/10.3945/AN.112.003491