- A study on mice published in Brain Behavior and Immunity found that Lactobacillus bacteria living in the gut protect against developing anxiety- and depression-like symptoms after stress exposure.
- Anxiety- and depression-like symptoms could be induced in mice not exposed to stress by transplanting gut microbiota from stressed mice
- Gut Lactobacillus bacteria increased the quantities of the interferon-gamma protein, which reduced neural reactions to stress.
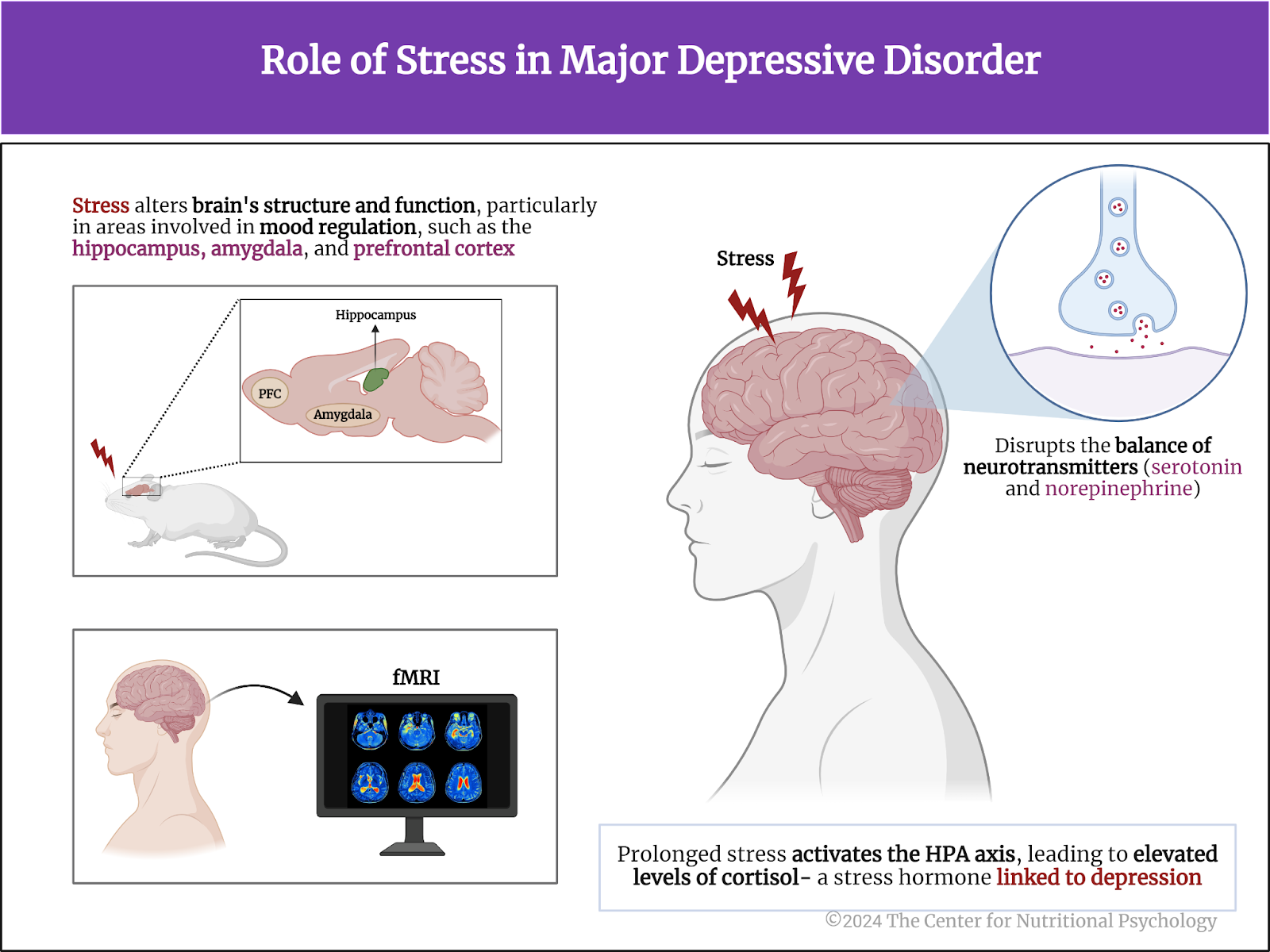
When we notice something really harmful, threatening, or challenging is happening, we experience a series of emotional states that prepare us to deal with that event. We may experience fear or anxiety, but we can also experience rage. If the developments threaten someone we love, our mind will remind us of that love and the need to act to protect that person. In such situations, our bodies will experience stress. The reactions will not be solely psychological, but a series of strong physiological changes will also occur.
What is stress?
Stress is the body’s natural response to perceived threats or challenges. It activates the body’s fight-or-flight response, releasing hormones like cortisol and adrenaline, which prepare the body to react to stressful situations. Short-term stress can be beneficial because it enhances focus and the body’s ability to withstand exertion and hardship. However, chronic stress can lead to various health problems, including anxiety, depression, and cardiovascular issues (McEwen, 2017; Tafet & Bernardini, 2003; Torpy et al., 2007).
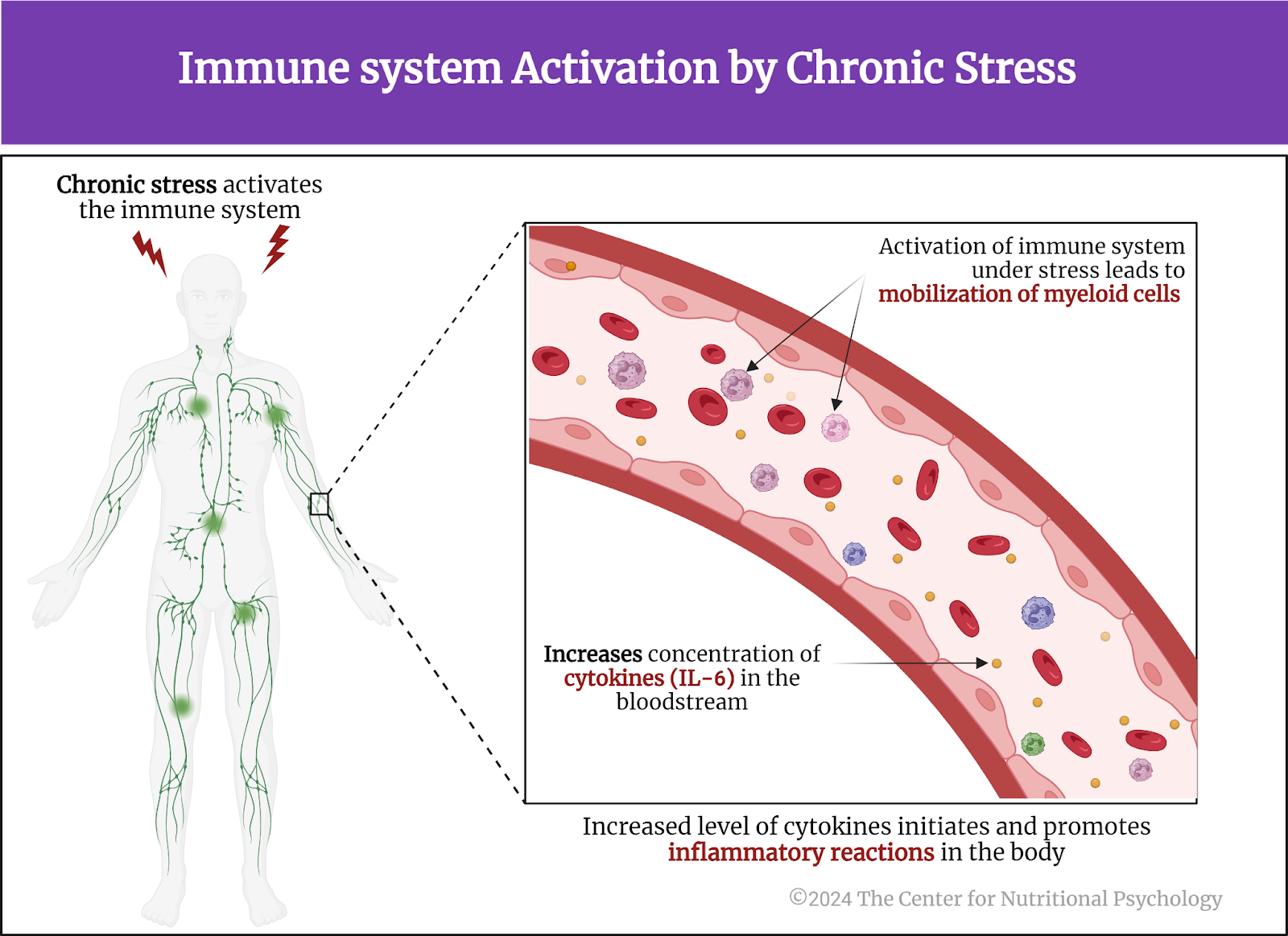
Studies have also linked chronic stress with the dysregulation of the immune system. Chronic stress is associated with a state of chronic low-grade inflammation that results in delayed wound healing and increased susceptibility to infectious illnesses (Gouin, 2011). The recent discovery of the microbiota-gut-brain axis (MGBA) has led to a stream of research implicating microorganisms living in the gut in the changes that develop due to chronic stress (Hedrih, 2023; Zhu et al., 2023).
The recent discovery of the MGBA has led to research implicating microorganisms living in the gut in the changes that develop due to chronic stress
The microbiota-gut-brain axis
The microbiota-gut-brain axis is a bidirectional communication pathway linking gut microbiota, i.e., the microorganisms living in the human gastrointestinal tract, with the brain. Through this pathway, gut microbiota can influence brain function and behavior and vice versa. This communication is achieved through mechanisms that are part of the nervous system and immune system, but also through hormones (García-Cabrerizo et al., 2021; Hedrih, 2023; Heiss et al., 2021).
Studies often report finding disruptions in the gut microbiota of individuals experiencing intensive stress or mood disorders (Merchak et al., 2024; Valles-Colomer et al., 2019) (see Figure 1).

Figure 1. Microbiota-gut-brain axis pathway
Studies often report finding disruptions in the gut microbiota of individuals experiencing intensive stress or mood disorders
Very often, there tend to be less Lactobacillus bacteria in the guts of these individuals. Also, studies on animals indicate that gut Lactobacillus bacteria aid stress resistance (Merchak et al., 2024)
The current study
Study author Andrea R. Merchak and her colleagues wanted to explore how completely removing Lactobacillus bacteria from mice’s guts would affect their behavior and specific metabolic processes. They used a set of eight bacterial strains known as the Altered Schaedler Flora to achieve this.
The Altered Schaedler Flora (ASF) consists of two strains of Lactobacillus, two strains of Clostridium, and one strain of Bacteroides, Mucispirillum, Eubacterium, and Pseudoflavonifactor. This set of bacterial species colonizes the guts of mice used in research, revealing the composition of their gut microbiota.
The study was conducted on four different groups of mice: a strain without gut microbiota (germ-free mice), a strain with Altered Schaedler Flora (ASF), a strain with the same flora but without Lactobacillus bacteria, and a group of standard laboratory mice (C57BL/6J).
Transferring gut microbiota from stressed mice to germ-free mice induced depressive- and anxiety-like symptoms
Some of the mice were exposed to unpredictable chronic stress during the experiments. Researchers would restrain them for two hours each day, but at different times, and apply one of three randomly chosen stressors each night—wet bedding, tilted cage, or two cage changes in a day. These mice developed symptoms similar to anxiety and depression in humans. As expected, they also had lower levels of gut Lactobacillus bacteria.
Researchers then transferred these mice’s dirty bedding to germ-free mice’s cages to transfer their gut microbiota. After this, the previously germ-free mice also developed anxiety—and depression-like behaviors, even though they were not exposed to stress. Further analyses revealed that these microbiota from stressed mice suppressed the production of interferon-gamma (IFNγ), an important signaling protein involved in the immune response (see Figure 2).

Figure 2. Study Procedure (Merchake et al., 2024)
Mice without Lactobacillus are more susceptible to stress
Study authors exposed some of the ASF mice with and without Lactobacillus bacteria in their guts to mild stress – being restrained in small vials with breathing holes for 3 hours. After this treatment, they analyzed the activity level in their brains during that period (using c-Fos staining after euthanizing the mice). They found that mice without gut Lactobacillus bacteria had increased activity in regions of the brain associated with fear and anxiety (the amygdala and the paraventricular thalamus) compared to mice with these bacteria (see Figure 3).

Figure 3. Link of Lactobacillus with stress
Mice without gut Lactobacillus bacteria had increased activity in regions of the brain associated with fear and anxiety
Interferon-gamma protects against the harmful effects of stress
They conducted another, somewhat different, experiment to verify this finding, and it also confirmed that mice without Lactobacillus bacteria are more susceptible to stress. Finally, the study authors conducted an experiment in which they administered interferon-gamma to one group of mice and antibodies to neutralize interferon-gamma to the other before exposing them to acute stress. Analysis of the brains of these mice showed that mice that received interferon-gamma had lower, while those who received the antibodies for it had higher levels of neural activity in brain regions responsible for fear and anxiety.
Mice without Lactobacillus bacteria are more susceptible to stress
Conclusion
The study showed that Lactobacillus bacteria seem to have a protective effect against developing anxiety—and depression-like symptoms after stress in mice. These bacteria seem to regulate the levels of the signaling protein interferon-gamma, which, in turn, reduces the anxiety—and depression-like effects of stress.
While humans and mice are very different species, they share many physiological similarities. If these findings are confirmed in humans, this might open ways to develop resilience to stress through interventions aimed at gut microbiota and diet.
The paper “Lactobacillus from the Altered Schaedler Flora maintain IFNγ homeostasis to promote behavioral stress resilience” was authored by Andrea R. Merchak, Samuel Wachamo, Lucille C. Brown, Alisha Thakur, Brett Moreau, Ryan M. Brown, Courtney R. Rivet-Noor, Tula Raghavan, and Alban Gaultier.
References
García-Cabrerizo, R., Carbia, C., O´Riordan, K. J., Schellekens, H., & Cryan, J. F. (2021). Microbiota-gut-brain axis as a regulator of reward processes. Journal of Neurochemistry, 157(5), 1495–1524. https://doi.org/10.1111/JNC.15284
Gouin, J.-P. (2011). Chronic Stress, Immune Dysregulation, and Health. American Journal of Lifestyle Medicine, 5(6), 476–485. https://doi.org/10.1177/1559827610395467
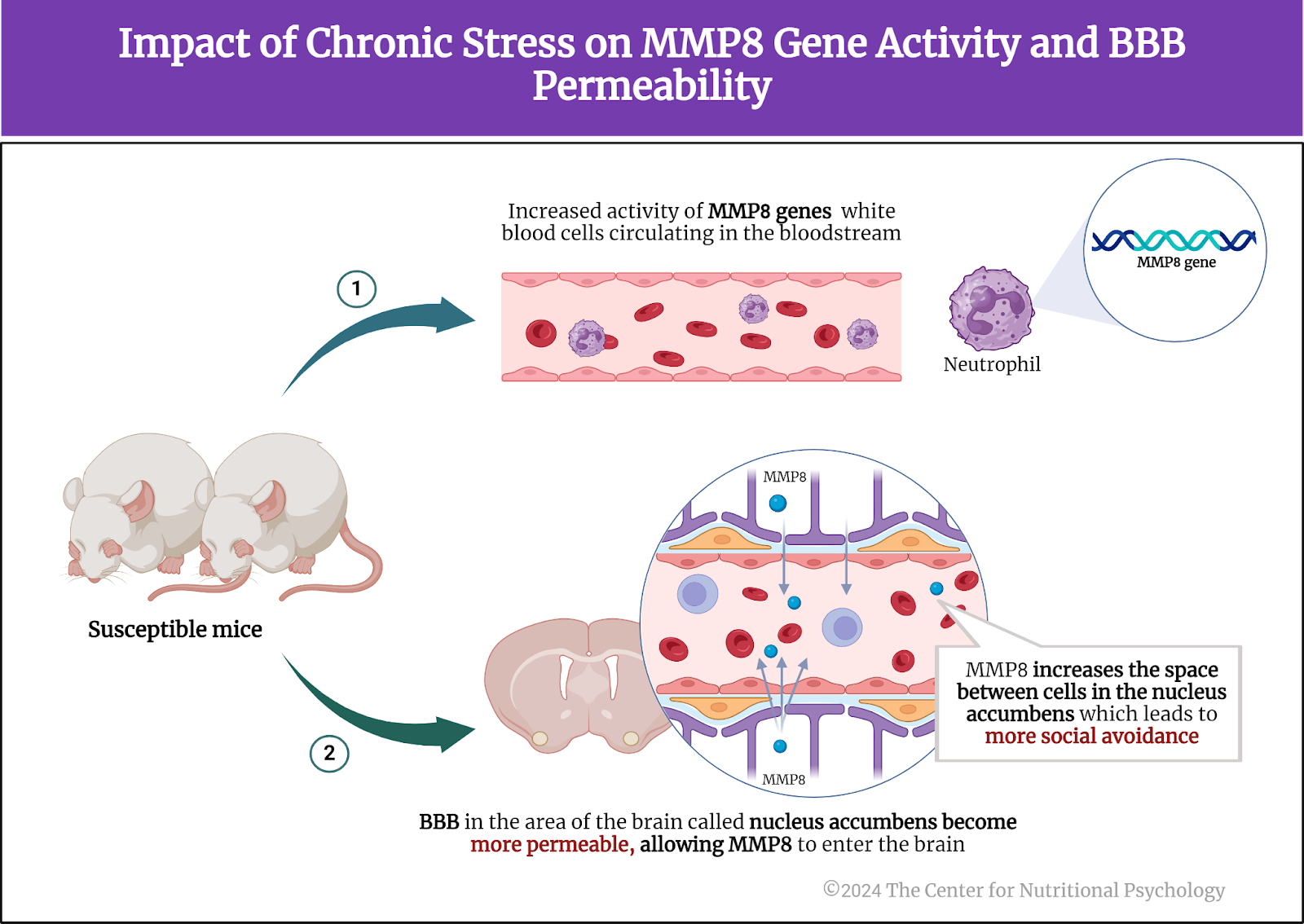
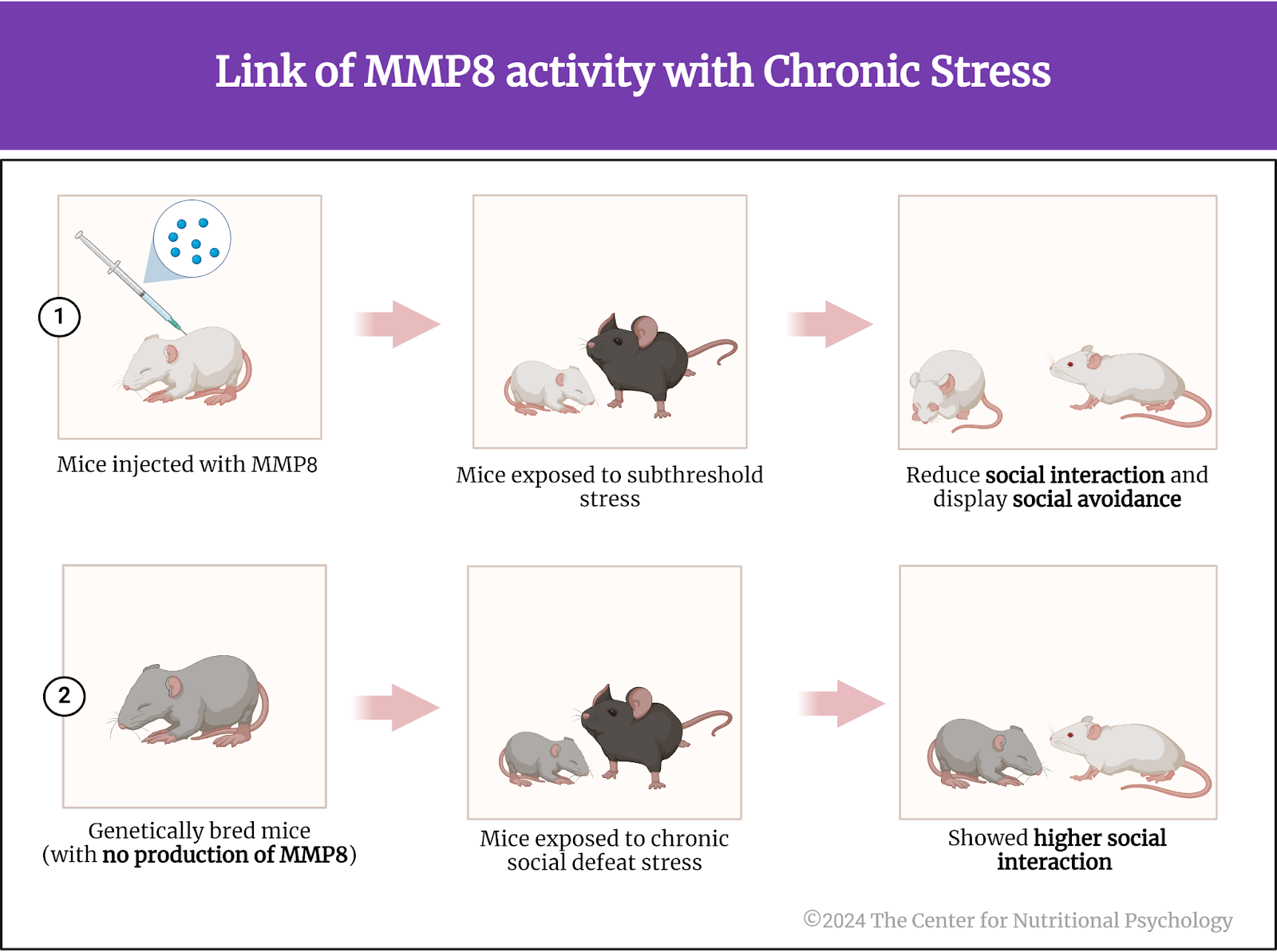
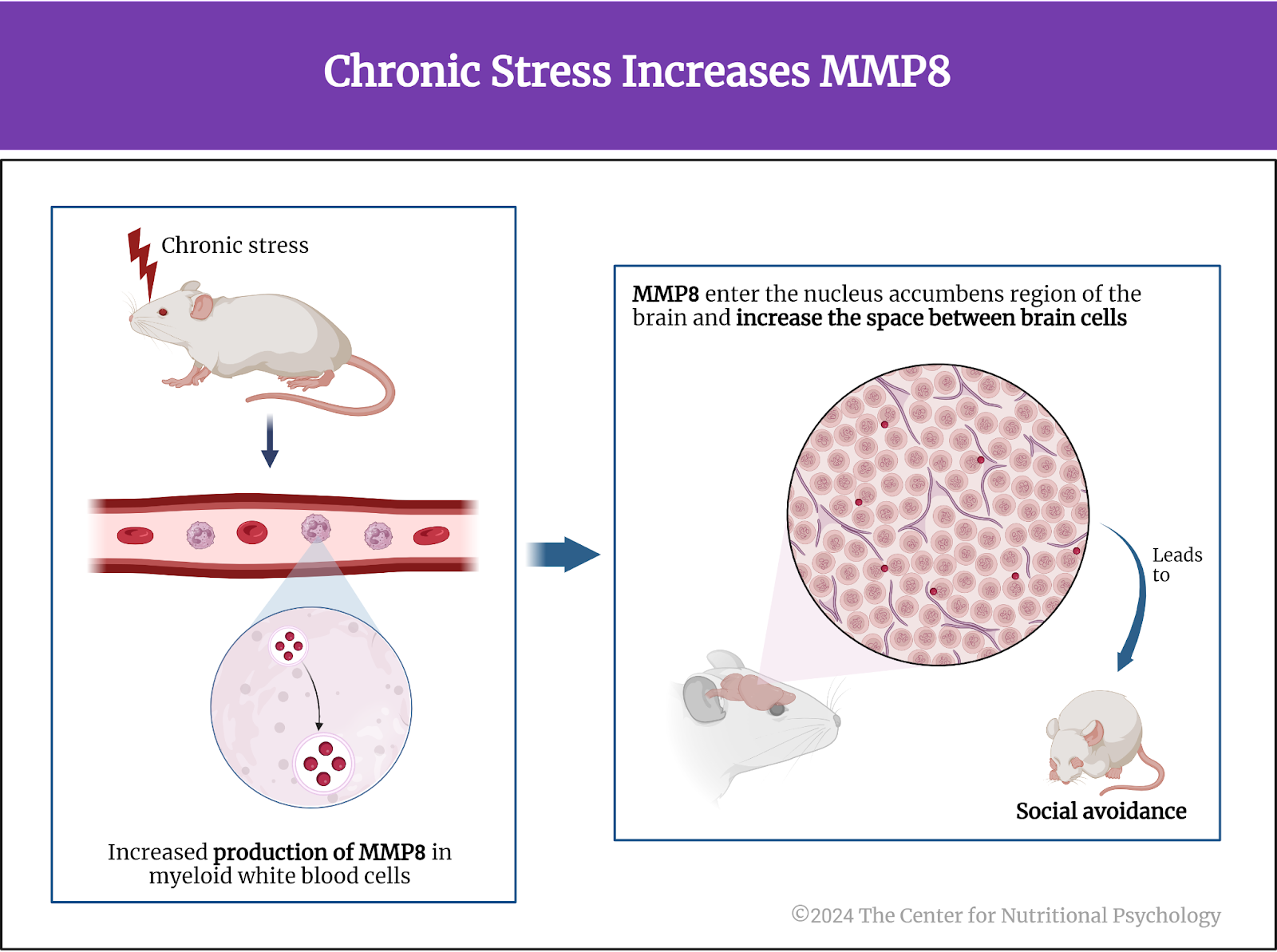
Hedrih, V. (2023). Immune Mechanism Linking Changes in Gut Microorganism and Behavior after Chronic Stress. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/researchers-discover-immune-mechanism-linking-changes-in-gut-microorganisms-and-behavior-after-chronic-stress/
Heiss, C. N., Mannerås-Holm, L., Lee, Y. S., Serrano-Lobo, J., Håkansson Gladh, A., Seeley, R. J., Drucker, D. J., Bäckhed, F., & Olofsson, L. E. (2021). The gut microbiota regulates hypothalamic inflammation and leptin sensitivity in Western diet-fed mice via a GLP-1R-dependent mechanism. Cell Reports, 35(8). https://doi.org/10.1016/j.celrep.2021.109163
McEwen, B. S. (2017). Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress, 1. https://doi.org/10.1177/2470547017692328
Merchak, A. R., Wachamo, S., Brown, L. C., Thakur, A., Moreau, B., Brown, R. M., Rivet-Noor, C. R., Raghavan, T., & Gaultier, A. (2024). Lactobacillus from the Altered Schaedler Flora maintain IFNγ homeostasis to promote behavioral stress resilience. Brain, Behavior, and Immunity, 115, 458–469. https://doi.org/10.1016/j.bbi.2023.11.001
Tafet, G. E., & Bernardini, R. (2003). Psychoneuroendocrinological links between chronic stress and depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27(6), 893–903. https://doi.org/10.1016/S0278-5846(03)00162-3
Torpy, J. M., Lynm, C., & Glass, R. M. (2007). Chronic Stress and the Heart. JAMA, 298(14), 1722. https://doi.org/10.1001/jama.298.14.1722
Valles-Colomer, M., Falony, G., Darzi, Y., Tigchelaar, E. F., Wang, J., Tito, R. Y., Schiweck, C., Kurilshikov, A., Joossens, M., Wijmenga, C., Claes, S., Van Oudenhove, L., Zhernakova, A., Vieira-Silva, S., & Raes, J. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology, 4(4), 623–632. https://doi.org/10.1038/s41564-018-0337-x
Zhu, X., Sakamoto, S., Ishii, C., Smith, M. D., Ito, K., Obayashi, M., Unger, L., Hasegawa, Y., Kurokawa, S., Kishimoto, T., Li, H., Hatano, S., Wang, T. H., Yoshikai, Y., Kano, S. ichi, Fukuda, S., Sanada, K., Calabresi, P. A., & Kamiya, A. (2023). Dectin-1 signaling on colonic γδ T cells promotes psychosocial stress responses. Nature Immunology. https://doi.org/10.1038/s41590-023-01447-8













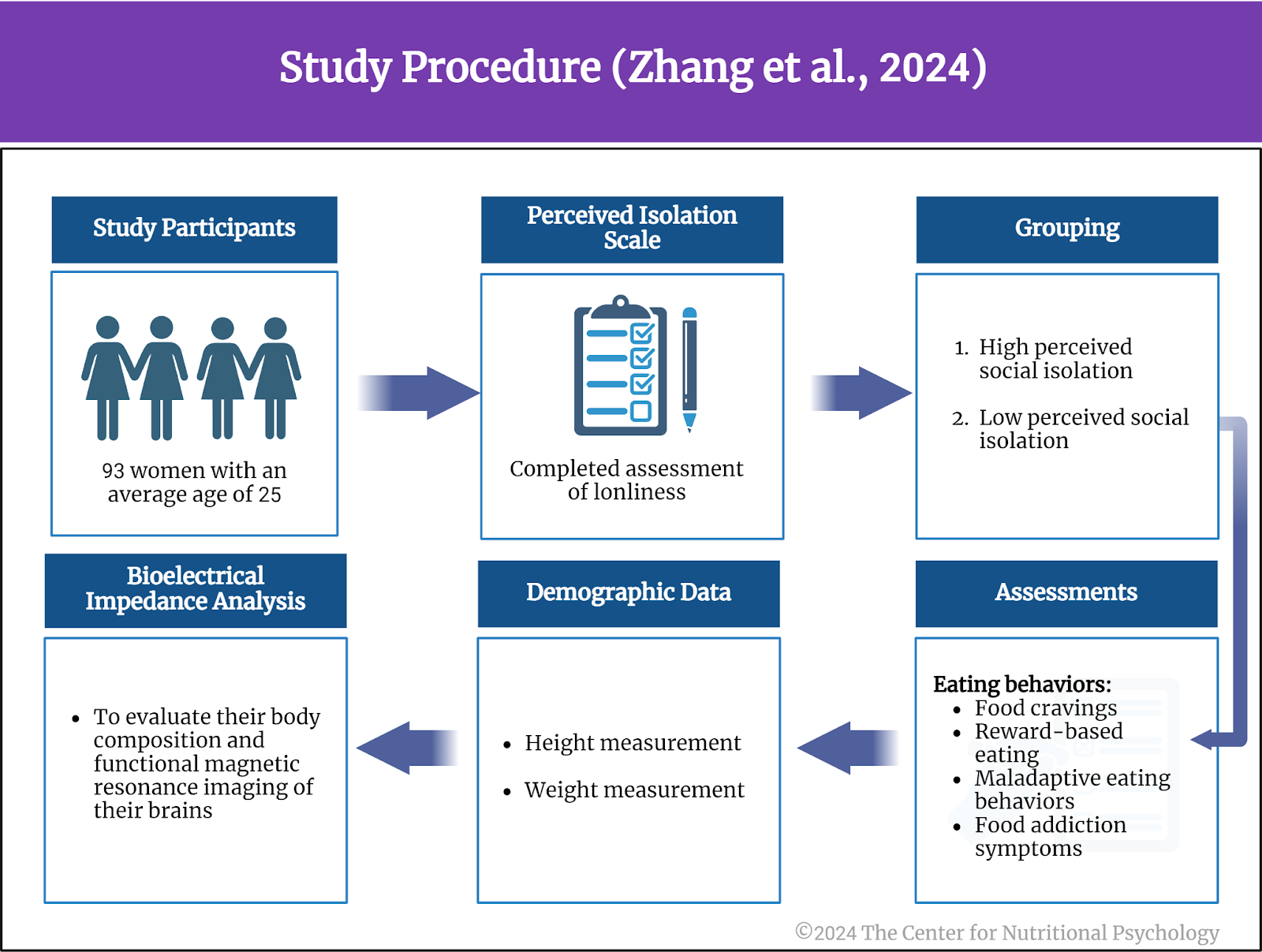
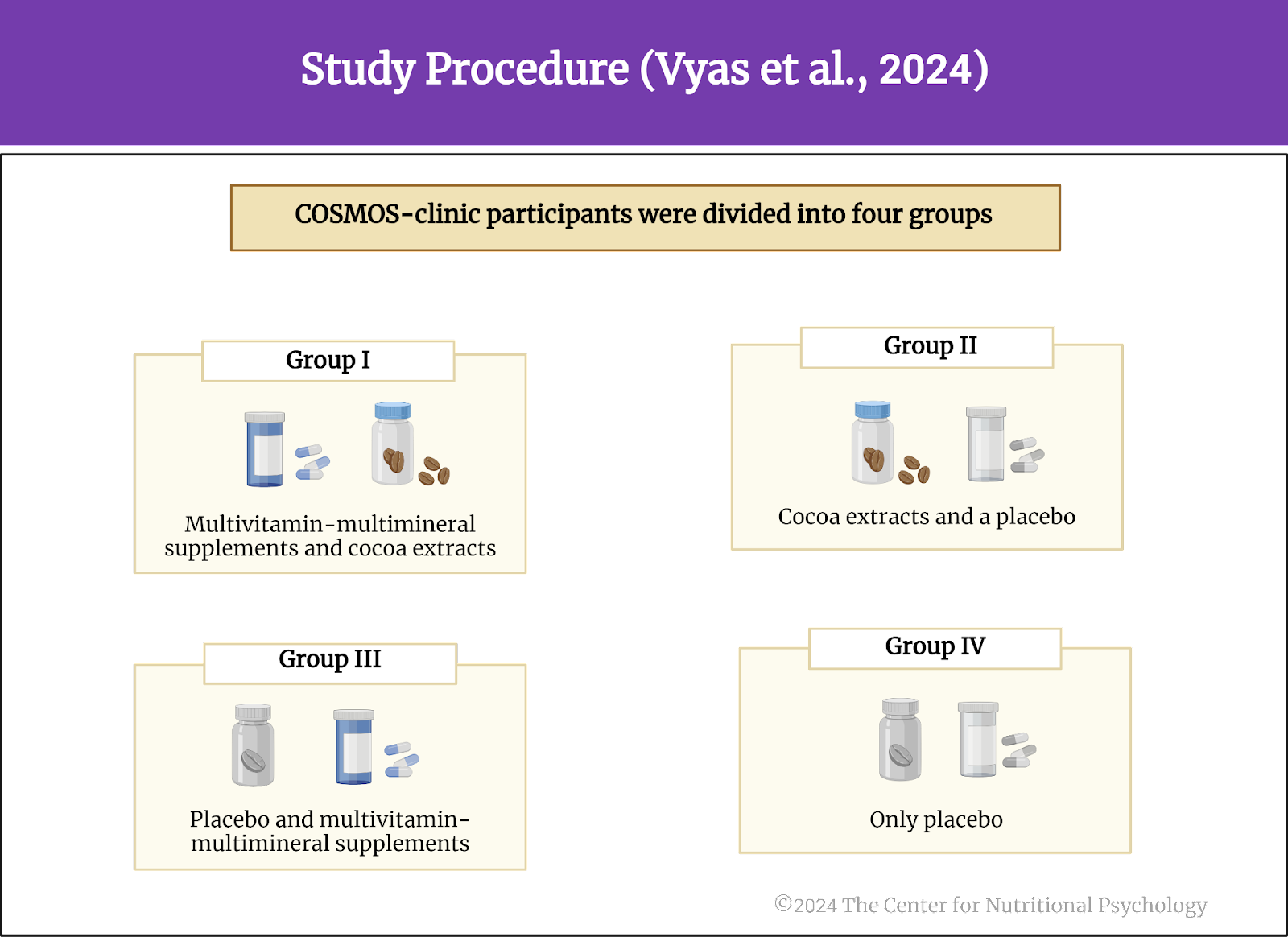
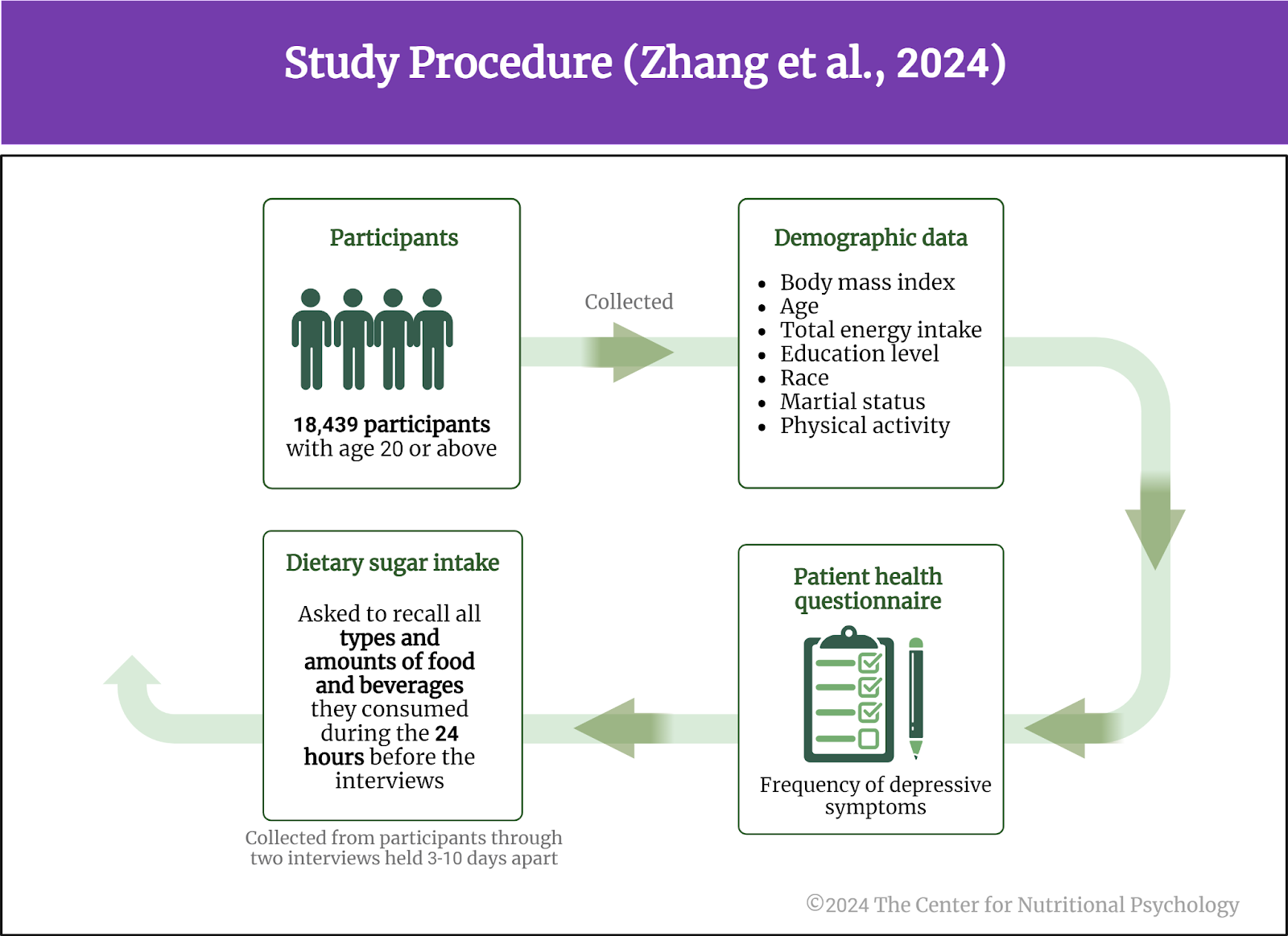
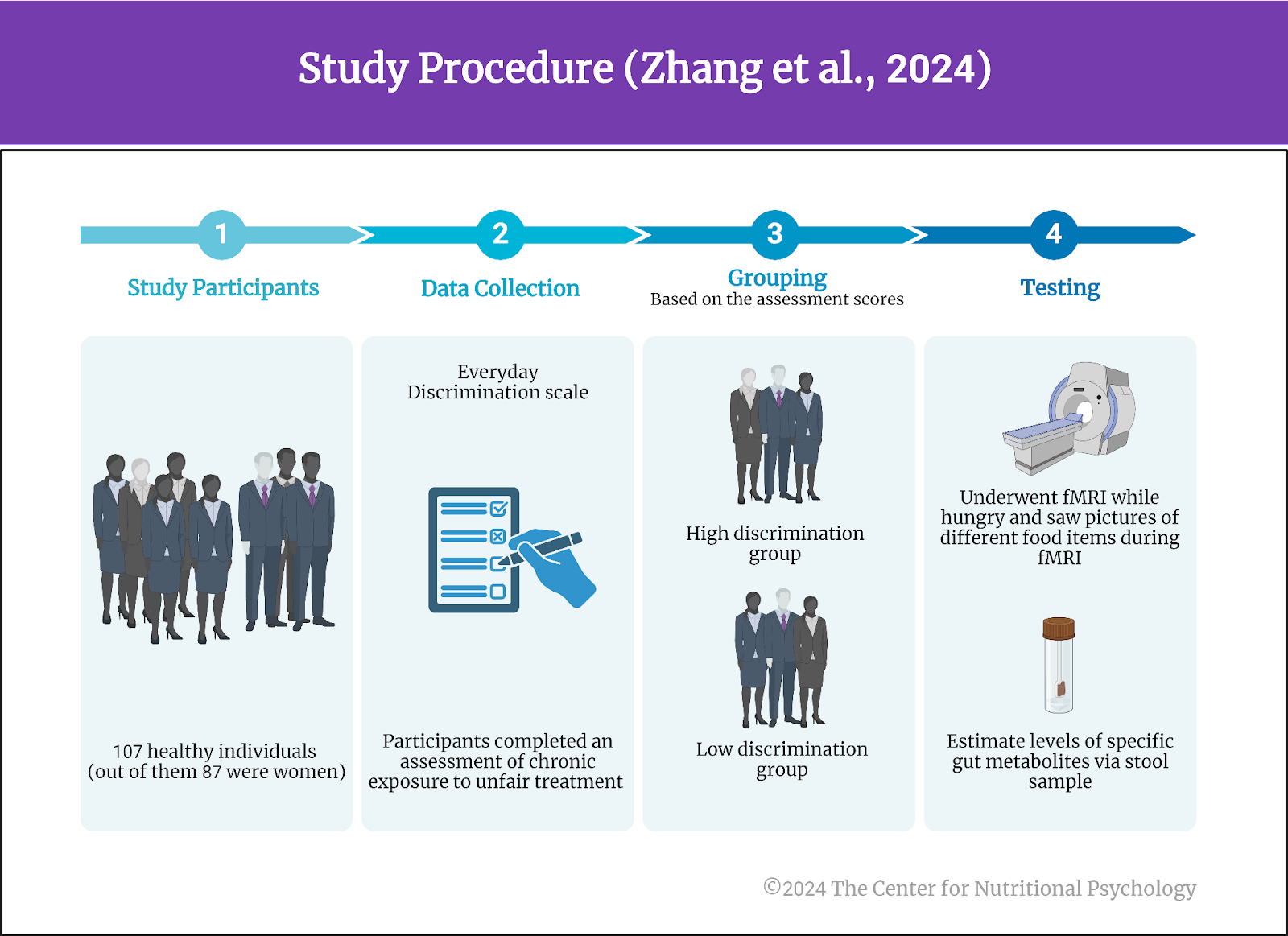 Figure 1. Study Procedure (Zhang et al., 2024)
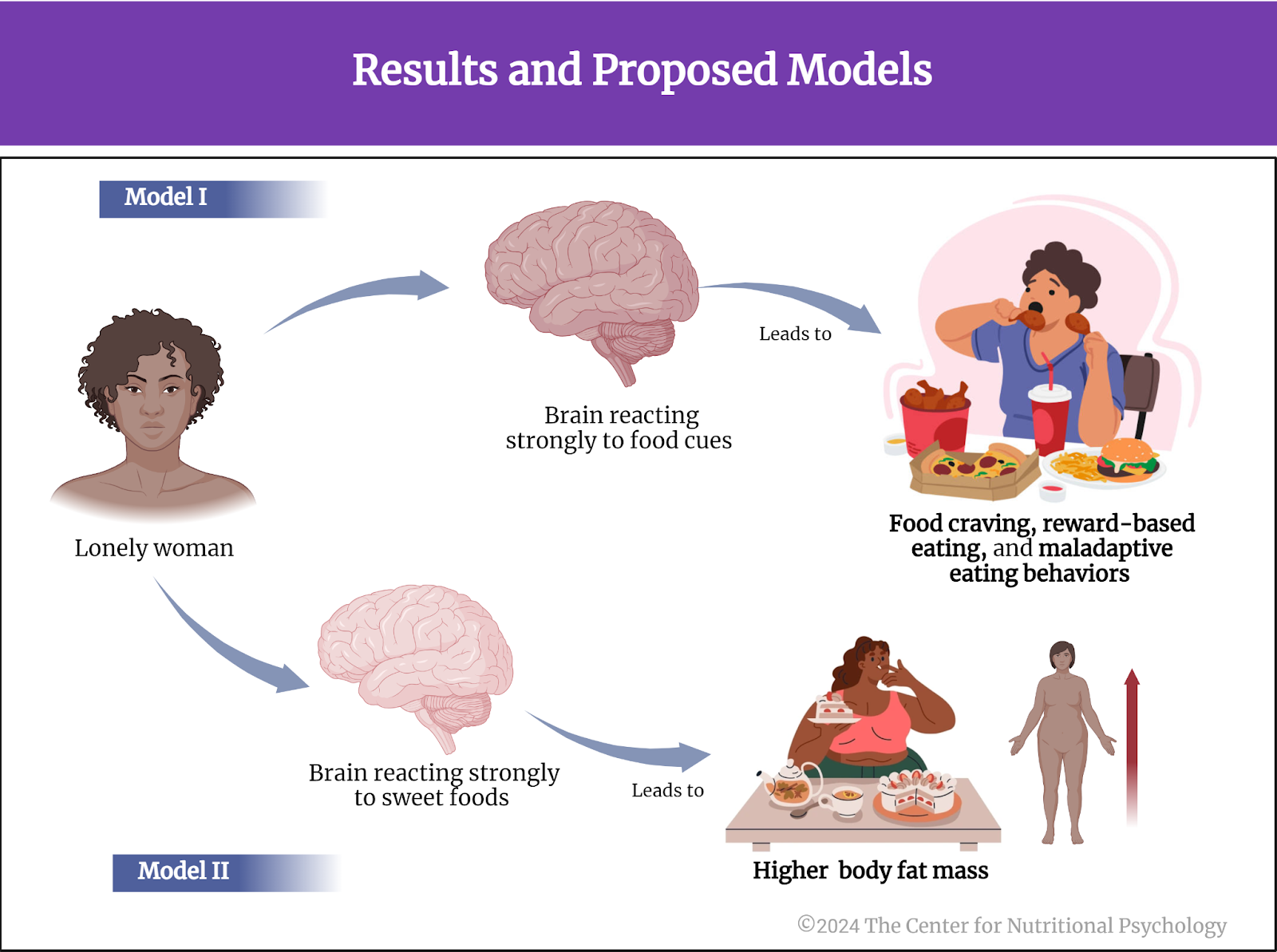
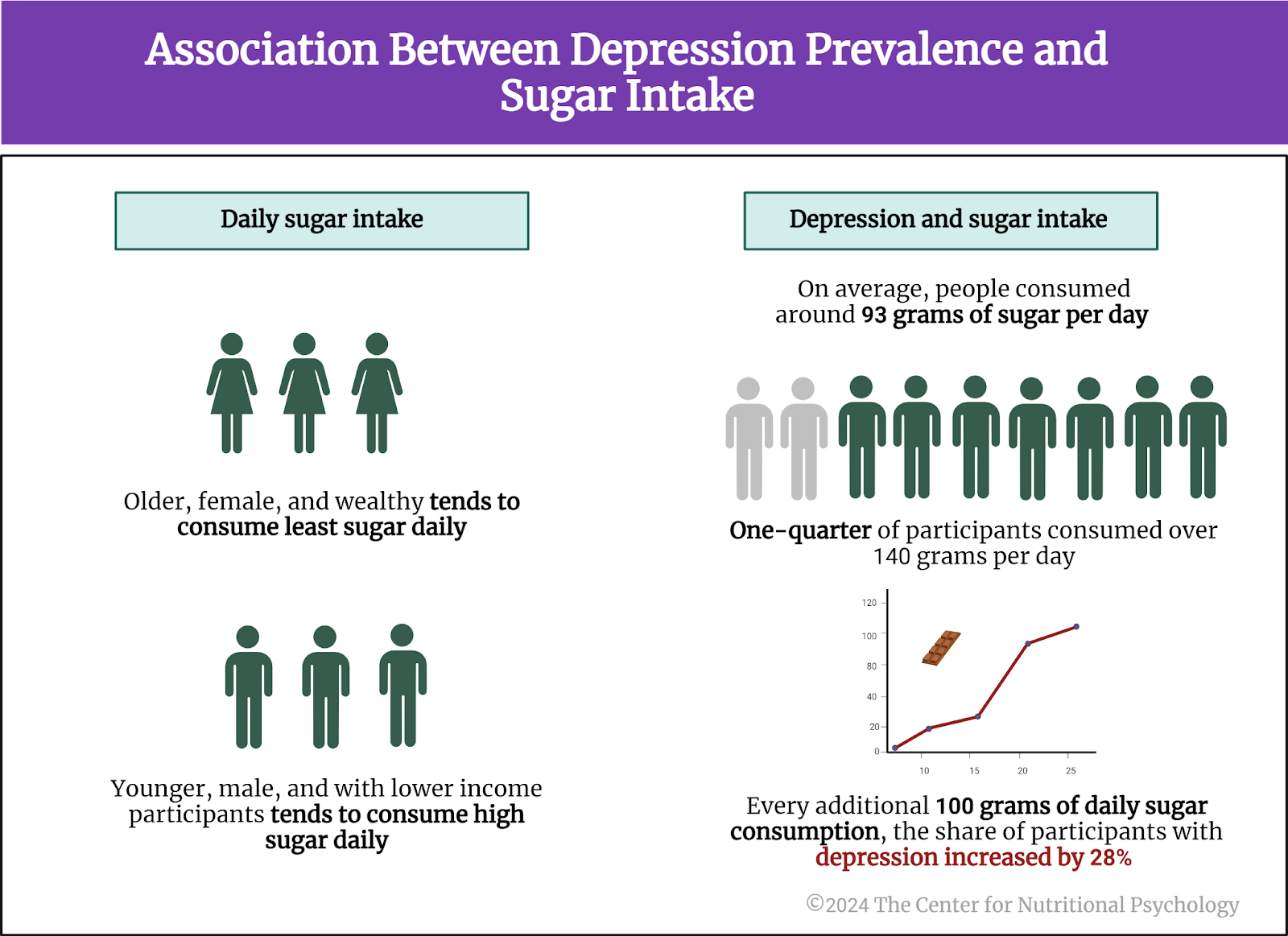
Figure 1. Study Procedure (Zhang et al., 2024)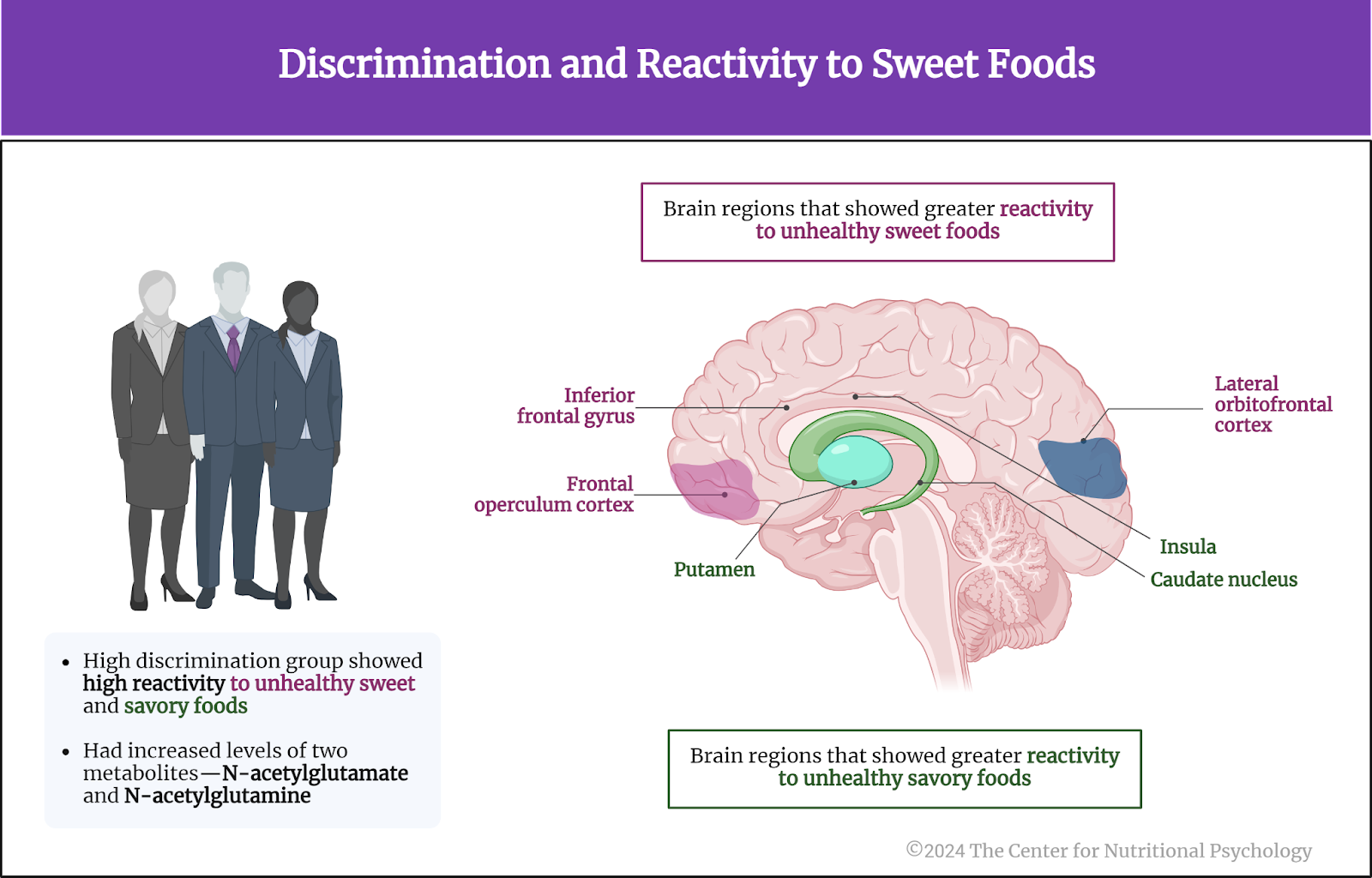 Figure 2. Discrimination and reactivity to sweet foods
Figure 2. Discrimination and reactivity to sweet foods