Reactions in Our Immune System Can Lead to Behavioral Changes, Including Depression
Listen to this Article
An enzyme produced in white blood cells regulates some of the psychological symptoms of depression
- A study on mice published in Nature reported that an enzyme called matrix metalloproteinase 8 (MMP8) regulates the effects of stress on the symptoms of depression.
- MMP8 was increased in the blood serum of humans with major depressive disorder and mice exposed to chronic stress.
- Injecting mice with an appropriate dose of MMP8 promoted social avoidance.
- The results showcase how immune system reactions can affect the brain, leading to profound behavioral changes.
Scientists have studied mental health problems for centuries. However, for most of this time, their focus has solely been on psychological symptoms because the scientific know-how needed to understand the complex biochemical mechanisms underpinning psychology was simply not there until now. Recent advances in biomedical technology allowed modern researchers to start mapping the biochemical mechanisms behind these disorders. One major topic of this type of research is stress-related disorders, such as major depressive disorder.
Major depressive disorder and stress
Major depressive disorder, or MDD, is a serious mental health condition characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities, often accompanied by physical symptoms such as changes in appetite or sleep patterns. It is one of the most frequent psychiatric disorders worldwide (Steffen et al., 2020; Weinberger et al., 2018).
Stress likely plays a significant role in the development and exacerbation of major depressive disorder
Studies on mice showed that chronic stress can lead to depression-like symptoms and alterations in the brain’s structure and function, particularly in areas involved in mood regulation, such as the hippocampus, amygdala, and prefrontal cortex (PFC) (Khan et al., 2020). Neuroimaging studies have reported alterations to similar brain areas in humans with depression (Zhang et al., 2018)
Stress can also disrupt the balance of neurotransmitters, like serotonin and norepinephrine, which are crucial for maintaining mood stability (Adell et al., 1988). Furthermore, prolonged stress activates the hypothalamic-pituitary-adrenal axis (HPA axis), leading to elevated cortisol levels. This stress hormone has been linked to depression (Tafet & Bernardini, 2003) (see Figure 1).
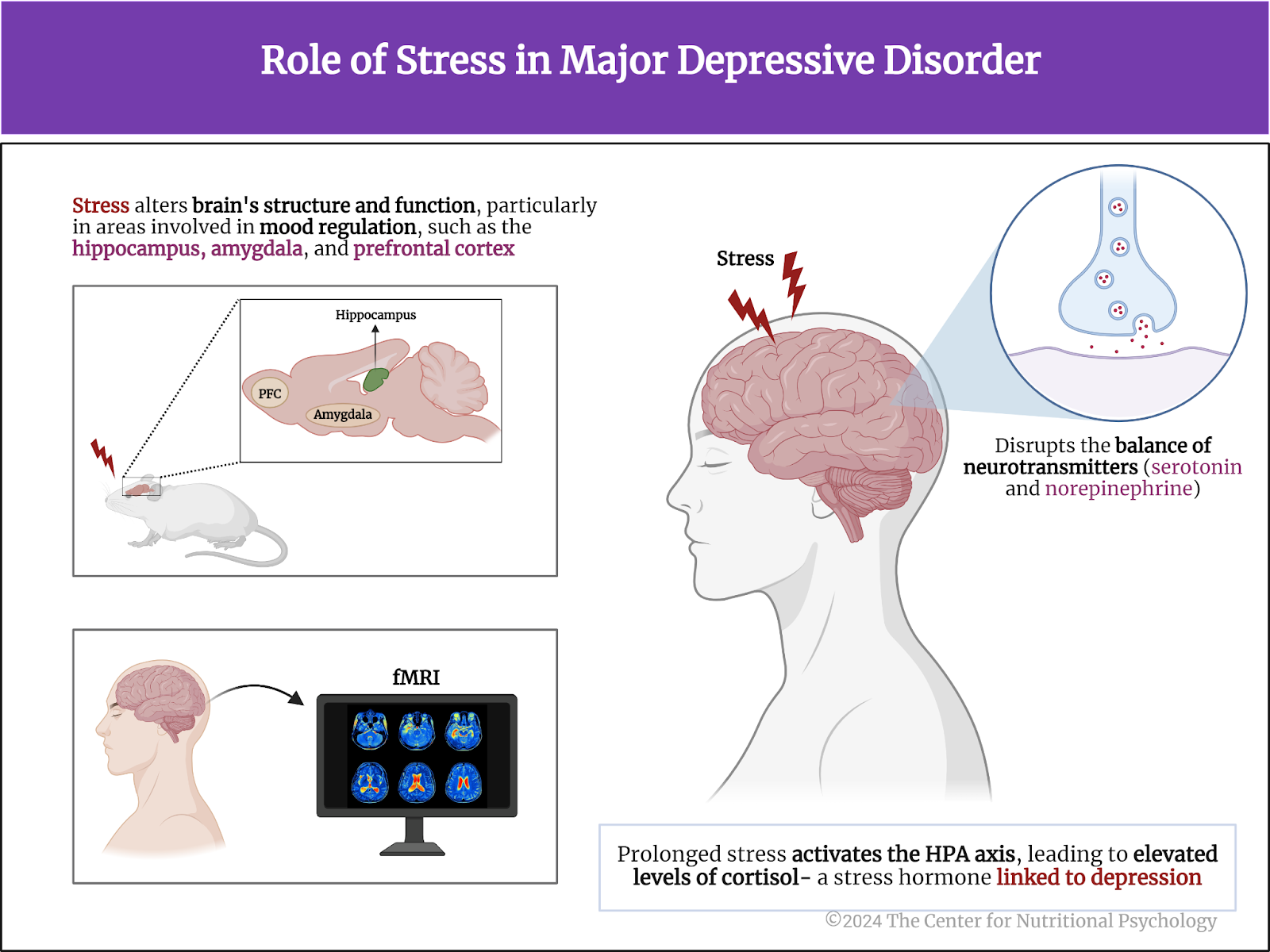
Figure 1. Role of stress in major depressive disorder
Inflammatory processes and depression
Studies show chronic stress also activates the immune system, the body’s natural defense against bacteria, viruses, and other pathogens. This activation leads to the mobilization of a type of white blood cell called myeloid cells. The organism under stress also increases the concentration of specific signaling proteins called cytokines (such as interleukin-6) in the bloodstream. This initiates and promotes inflammatory reactions in the body (Cathomas et al., 2024) (see Figure 2).
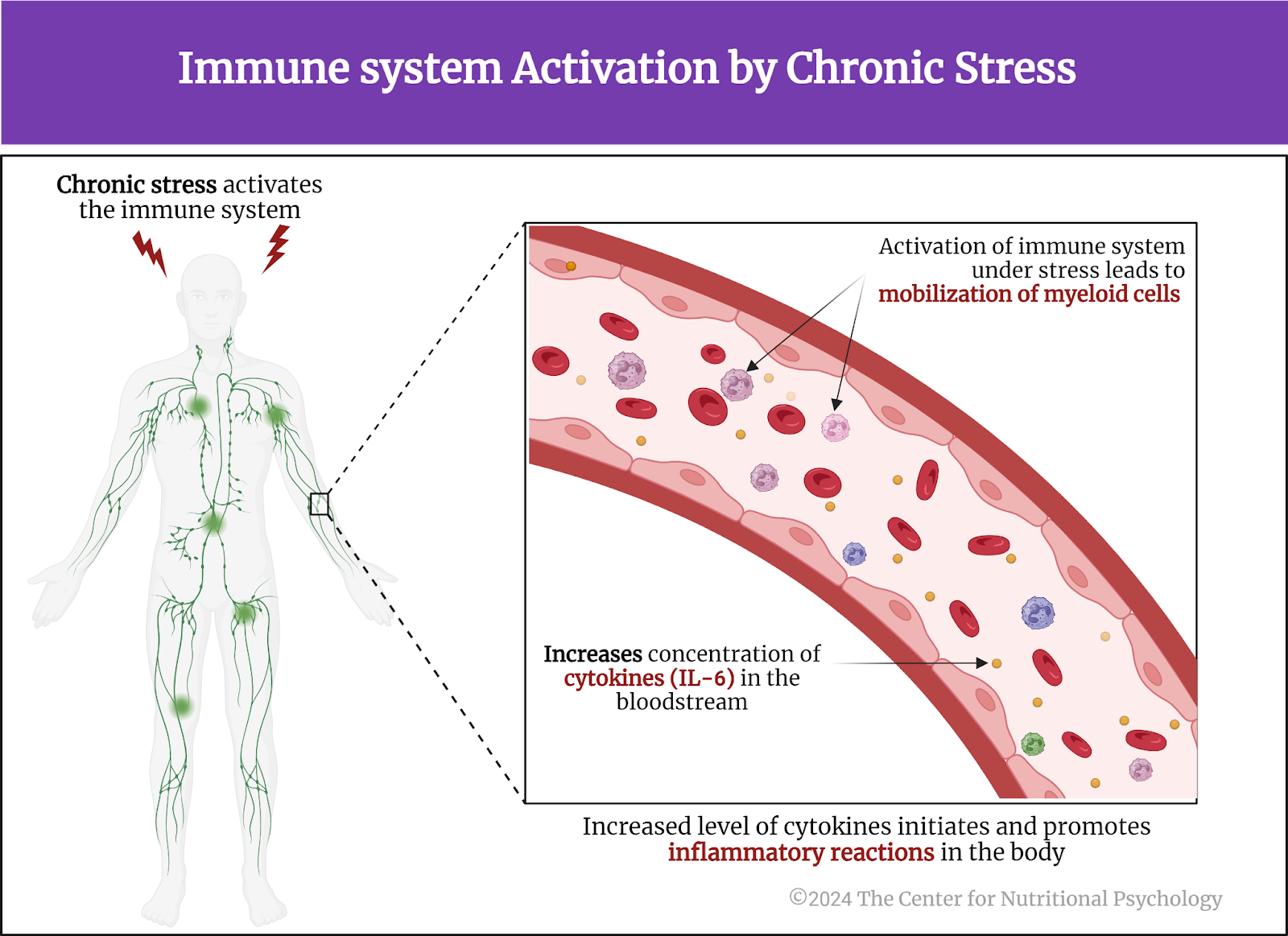
Figure 2. Immune system activation by chronic stress
In line with this, studies on humans show that individuals with stress-related mental health conditions such as major depressive disorder display a state of chronic low-grade inflammation characterized by increased concentrations of these pro-inflammatory proteins in the bloodstream (Dowlati et al., 2010)
The current study
Study author Flurin Cathomas and his colleagues wanted to understand better the role of immune system molecules in the development of psychological symptoms of depression. The initial results they obtained focused their attention on the role of the enzyme matrix metalloproteinase 8 (MMP8).
MMP8 belongs to the metalloproteinase family, a group of enzymes responsible for breaking down extracellular matrix proteins. MMP8 is primarily produced by neutrophils, a type of myeloid white blood cell that plays a crucial role in the immune system’s response to infection and inflammation. They are derived from myeloid progenitor cells in the bone marrow.
These researchers conducted experiments on 4-7-week-old mice purchased externally or bred in the researchers’ laboratory. In the experiments, the study authors exposed these mice to different types of stressors and conducted different biomedical and surgical procedures. The main type of stress-induced in these mice was chronic social defeat. This was done by exposing them for 5 or 10 minutes to a large, aggressive mouse for ten days. After this treatment, some mice started avoiding other mice, developing social avoidance, a pattern of behaviors comparable to that of depression in humans. Other mice did not. Study authors called the first type of mice “susceptible” mice and the later “resistant” mice. They also used mice not exposed to stress as controls (see Figure 3).

Figure 3. Study Procedure (Cathomas, 2024)
Chronic stress upregulates genes producing MMP8 in the bloodstream of susceptible mice
The study authors examined the activity of white blood cells in mice and grouped them into four categories based on their gene activity patterns. They identified a group of genes that were more active in susceptible mice compared to controls. Many of the genes in this group were proteins known to play a role in the process of inflammation. One of the most differentially active genes in the two groups of mice was the one encoding MMP8.
Further analysis showed that this increased activity of MMP8 genes was not found in the brain but only in white blood cells circulating in the bloodstream. Although these MMP8 molecules are produced outside the brain, it turned out that they can still travel to the brain. Chronic stress makes the blood-brain barrier (BBB) in the area of the brain called nucleus accumbens more permeable, allowing MMP8 to enter the brain at that point. Upon entering, they increase the space between cells in this area. A separate experiment showed that increasing the space between cells in the nucleus accumbens leads to more social avoidance in these mice (see Figure 4).
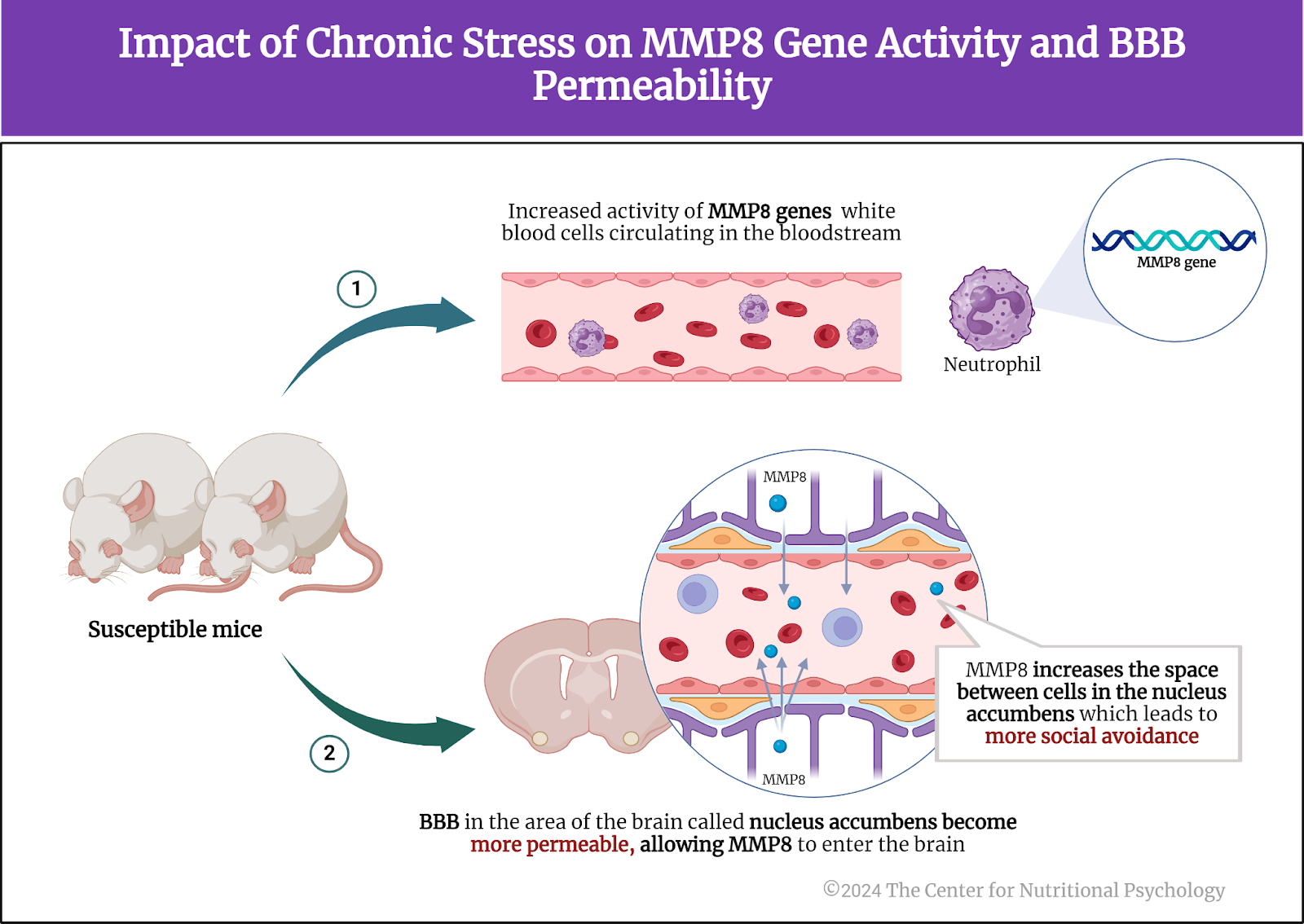
Figure 4. Impact of chronic stress on MMP8 gene activity and BBB permeability
Study authors verified these findings in humans and found that individuals with major depressive disorder also have increased concentrations of MMP8 in their bloodstream.
MMP8 regulates social avoidance
When study authors injected MMP8 into mice that were exposed to subthreshold stress (social defeat stress insufficient to produce behavioral changes), these mice also reduced their social interactions (i.e., started displaying social avoidance). To ensure this is the effect of MMP8 (and not of something else), the study authors bred mice genetically altered not to produce it. Exposing these mice to chronic social defeat stress did not result in social avoidance. They even showed higher social interaction and spent less time in the corner than regular mice. This indicated that MMP8 regulates social avoidance behavior in mice (Figure 5).
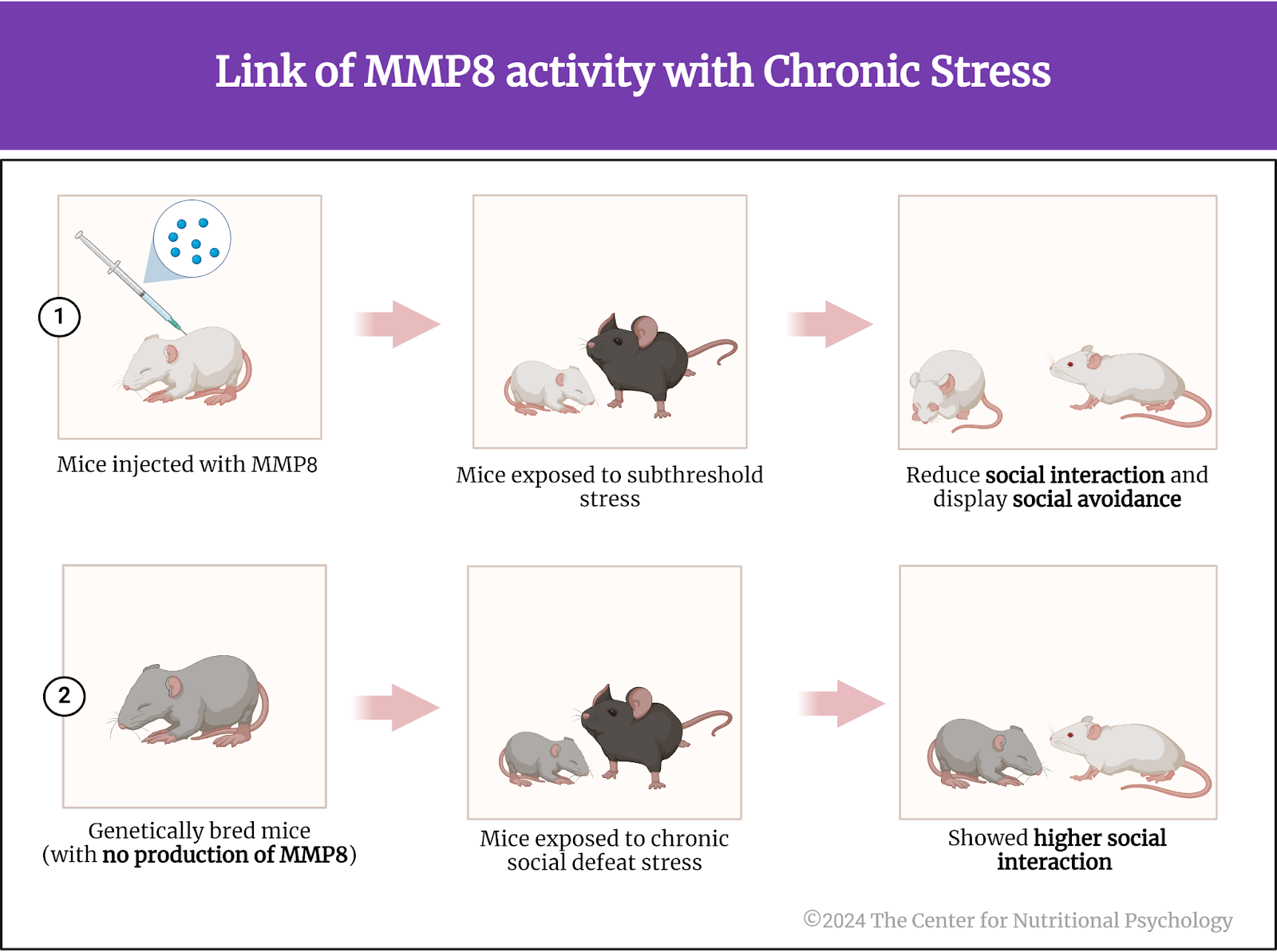
Figure 5. Link of MMP8 activity with chronic stress
Conclusion
The study showed that chronic stress increases the enzyme matrix metalloproteinase 8 (MMP8) production in myeloid white blood cells in the bloodstream. These enzymes enter the nucleus accumbens region of the brain and increase the space between brain cells, leading to social avoidance in mice (see Figure 6).
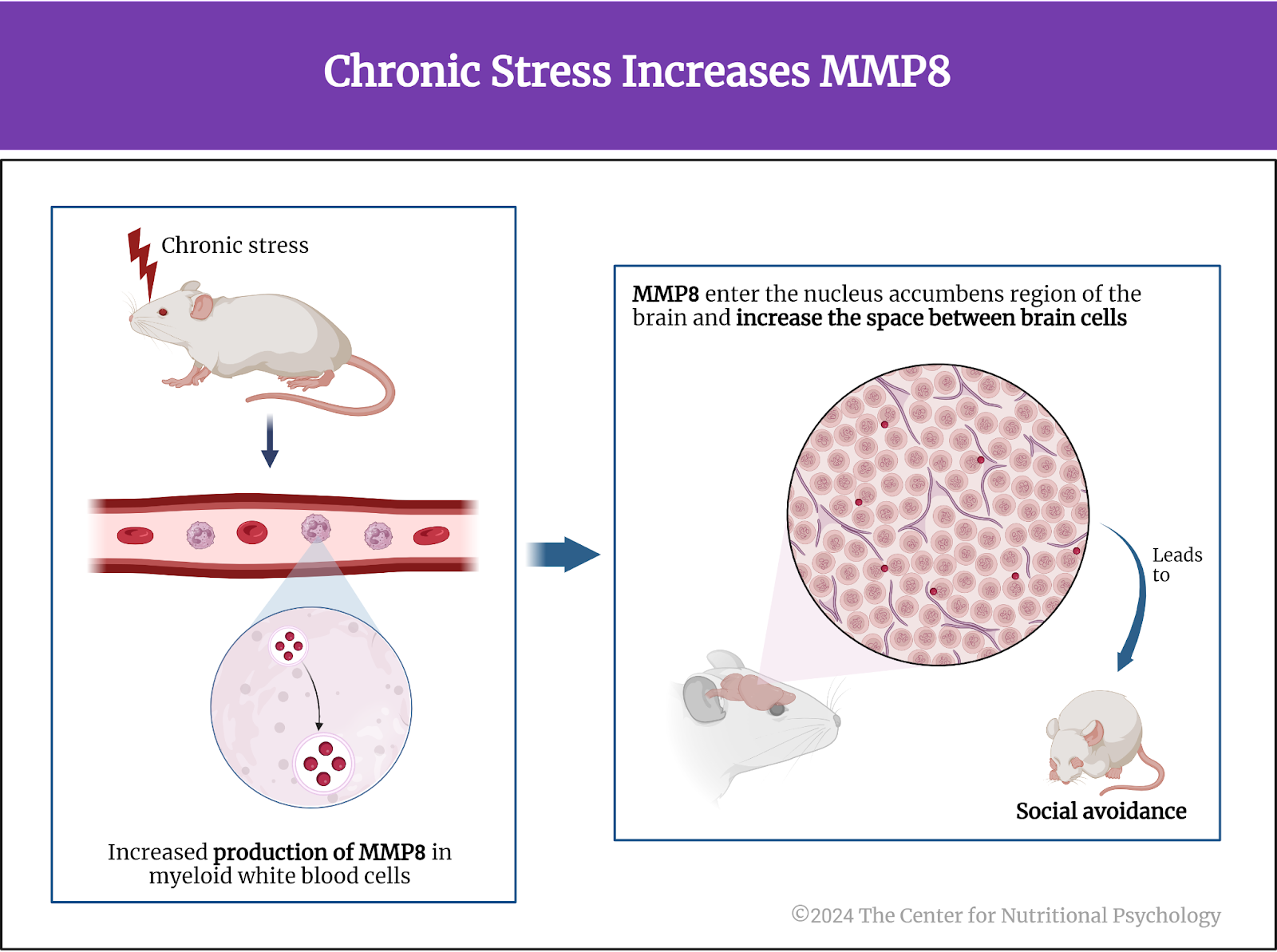
Figure 6. Chronic stress increases MMP8
Although the study was conducted on mice, similar physiological mechanisms also likely exist in humans. Thanks to this similarity, these findings contribute to the scientific understanding of biochemical mechanisms underpinning psychological reactions to chronic stress and symptoms of disorders such as depression. Understanding the biochemical mechanisms of mental disorders will likely lead to the development of much more effective ways to treat them.
The paper “Circulating myeloid-derived MMP8 in stress susceptibility and depression” was authored by Flurin Cathomas, Hsiao-Yun Lin, Kenny L. Chan, Long Li, Lyonna F. Parise, Johana Alvarez, Romain Durand-de Cuttoli, Antonio V. Aubry, Samer Muhareb, Fiona Desland, Yusuke Shimo, Aarthi Ramakrishnan, Molly Estill, Carmen Ferrer-Pérez, Eric M. Parise, C. Matthias Wilk, Manuella P. Kaster, Jun Wang, Allison Sowa, William G. Janssen, Sara Costi, Adeeb Rahman, Nicolas Fernandez, Matthew Campbell, Filip K. Swirski, Eric J. Nestler, Li Shen, Miriam Mera, James W. Murrough, and Scott J. Russo.
References
Adell, A., Garcia-Marquez, C., Armario, A., & Gelpi, E. (1988). Chronic Stress Increases Serotonin and Noradrenaline in Rat Brain and Sensitizes Their Responses to a Further Acute Stress. Journal of Neurochemistry, 50(6), 1678–1681. https://doi.org/10.1111/j.1471-4159.1988.tb02462.x
Cathomas, F., Lin, H.-Y., Chan, K. L., Li, L., Parise, L. F., Alvarez, J., Durand-de Cuttoli, R., Aubry, A. V., Muhareb, S., Desland, F., Shimo, Y., Ramakrishnan, A., Estill, M., Ferrer-Pérez, C., Parise, E. M., Wilk, C. M., Kaster, M. P., Wang, J., Sowa, A., … Russo, S. J. (2024). Circulating myeloid-derived MMP8 in stress susceptibility and depression. Nature, 626(8001), 1108–1115. https://doi.org/10.1038/s41586-023-07015-2
Dowlati, Y., Herrmann, N., Swardfager, W., Liu, H., Sham, L., Reim, E. K., & Lanctôt, K. L. (2010). A Meta-Analysis of Cytokines in Major Depression. Biological Psychiatry, 67(5), 446–457. https://doi.org/10.1016/j.biopsych.2009.09.033
Khan, A. R., Geiger, L., Wiborg, O., & Czéh, B. (2020). Stress-Induced Morphological, Cellular and Molecular Changes in the Brain—Lessons Learned from the Chronic Mild Stress Model of Depression. Cells, 9(4), 1026. https://doi.org/10.3390/cells9041026
Steffen, A., Thom, J., Jacobi, F., Holstiege, J., & Bätzing, J. (2020). Trends in prevalence of depression in Germany between 2009 and 2017 based on nationwide ambulatory claims data. Journal of Affective Disorders, 271, 239–247. https://doi.org/10.1016/J.JAD.2020.03.082
Tafet, G. E., & Bernardini, R. (2003). Psychoneuroendocrinological links between chronic stress and depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27(6), 893–903. https://doi.org/10.1016/S0278-5846(03)00162-3
Weinberger, A. H., Gbedemah, M., Martinez, A. M., Nash, D., Galea, S., & Goodwin, R. D. (2018). Trends in depression prevalence in the USA from 2005 to 2015: Widening disparities in vulnerable groups. Psychological Medicine, 48(8), 1308–1315. https://doi.org/10.1017/S0033291717002781
Zhang, F.-F., Peng, W., Sweeney, J. A., Jia, Z.-Y., & Gong, Q.-Y. (2018). Brain structure alterations in depression: Psychoradiological evidence. CNS Neuroscience & Therapeutics, 24(11), 994–1003. https://doi.org/10.1111/cns.12835





Leave a comment