Whole Food Dietary Interventions to Improve Depression Symptoms
Depression is a debilitating mental illness that often manifests with physical symptoms such as fatigue and cognitive impairments. Globally, it is a prevalent disability that can be treated through a combination of evidence-based therapies and medications. While these are viable options for individuals seeking help, their general effectiveness across diverse populations has yet to be established and, importantly, may not be suitable for those whose symptoms make it difficult to pursue treatment consistently.
In seeking alternatives that are more feasible to implement in addressing chronic depression, numerous epidemiological studies have uncovered an inverse correlation between diet quality and depression (Molendijk et al., 2018; Lassale et al., 2019; Wu et al., 2020). Biological mechanisms—like inflammation, oxidation, and stress—have been proposed as drivers of depression, and diets enriched with polyphenol and omega-3 fatty acids have proved effective in improving depressive symptoms (Jang et al., 2020, Marx et al., 2020).
Numerous epidemiological studies have uncovered an inverse correlation between diet quality and depression.
However, the relationship between diet and mental health is difficult to elucidate as research mostly focuses on micronutrients, which humans do not eat in isolation (O’Neill et al., 2022). In an effort to clarify the positive impact of dietary interventions on depression, O’Neill et al. conducted a systematic review of clinical trials emphasizing the effects of whole food diets on depressive symptoms.
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Academy of Nutrition and Dietetics Quality Criteria (ANDQCC) Checklists, the authors reviewed results from randomized control trials (RCTs) in which only whole foods/diet dietary interventions were used to address depression (Page et al., 2021). PRISMA was utilized to ensure appropriate studies were included in the literature search and ANDQCC was leveraged to reduce the risk of bias in the selected studies by assessing their validity with a series of quality criteria questions. Moreover, the authors intentionally limited their reviews of RCTs from 2000 to 2021 to produce conclusions that better reflect today’s dietary landscape and the possible benefits of whole foods/diets in treating depression.
From a total of 3,030 studies, seven studies were ultimately included and analyzed in their systematic review, representing adult populations from the USA, the UK, Australia, and Korea. These studies utilized whole food interventions—characterized by the consumption of minimally processed foods—and/or whole diet interventions that carefully regulated dietary intake to evaluate how they improved depressive symptoms according to standardized depression measures (O’Neill et al., 2022).
Across all studies, these interventions reduced depressive symptoms and, in particular, whole diet interventions involving flavonoids led to the greatest decrease in depression scores. These phytochemicals are abundant in Mediterranean diets and have been demonstrated to alleviate depression through antioxidative and anti-inflammatory processes (Godos et al., 2018; Bayes et al., 2020; Ventriglio et al., 2020).
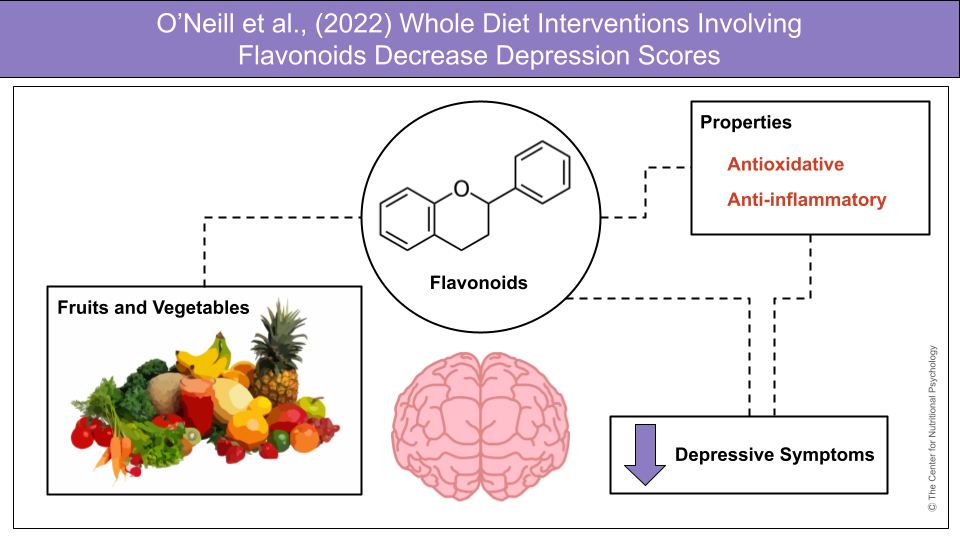
Figure 1. Whole diets rich in flavonoids were associated with lower depressive symptoms, most likely through antioxidative and anti-inflammatory effects, as reported through standardized depression scores.
Flavonoids are plant compounds that are obtainable through a diet rich in fruits and vegetables. There are six primary types of flavonoids, each with health-promoting anti-inflammatory effects, along with antioxidant properties which protect cells from oxidative damage. Flavonoids have been identified in the literature as natural antidepressants with additional benefits in reducing the risks of heart disease and diabetes (Hritcu et al., 2017; Pannu et al., 2021). Sources of flavonoids include dark leafy greens, vegetables, berries, seeds, nuts, beans, and grains.
Whole diet interventions involving flavonoids led to the greatest decrease in depression scores.
For more information on how plant compounds influence brain function and mental health, visit the Center for Nutritional Psychology (CNP) Nutritional Psychology Research Libraries (NPRLs).
References
Bayes, J., Schloss, J., & Sibbritt, D. (2020). Effects of Polyphenols in a Mediterranean Diet on Symptoms of Depression: A Systematic Literature Review. Advances in nutrition (Bethesda, Md.), 11(3), 602–615. https://doi.org/10.1093/advances/nmz117
Godos, J., Castellano, S., Ray, S., Grosso, G., & Galvano, F. (2018). Dietary Polyphenol Intake and Depression: Results from the Mediterranean Healthy Eating, Lifestyle and Aging (MEAL) Study. Molecules (Basel, Switzerland), 23(5), 999. https://doi.org/10.3390/molecules23050999
Gomez-Pinilla, F., Foster, J. A., Cani, P. D., Thuret, S., Staudacher, H. M., … Jacka, F. N. (2021). Diet and depression: exploring the biological mechanisms of action. Molecular psychiatry, 26(1), 134–150. https://doi.org/10.1038/s41380-020-00925-x
Hritcu, L., Ionita, R., Postu, P. A., Gupta, G. K., Turkez, H., Lima, T. C., Carvalho, C., & de Sousa, D. P. (2017). Antidepressant Flavonoids and Their Relationship with Oxidative Stress. Oxidative medicine and cellular longevity, 2017, 5762172. https://doi.org/10.1155/2017/5762172
Jang, S. H., Woo, Y. S., Lee, S. Y., & Bahk, W. M. (2020). The Brain-Gut-Microbiome Axis in Psychiatry. International journal of molecular sciences, 21(19), 7122. https://doi.org/10.3390/ijms21197122
Lassale, C., Batty, G. D., Baghdadli, A., Jacka, F., Sánchez-Villegas, A., Kivimäki, M., & Akbaraly, T. (2019). Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Molecular psychiatry, 24(7), 965–986. https://doi.org/10.1038/s41380-018-0237-8
Marx, W., Lane, M., Hockey, M., Aslam, H., Berk, M., Walder, K., Borsini, A., Firth, J., Pariante, C. M., Berding, K., Cryan, J. F., Clarke, G., Craig, J. M., Su, K. P., Mischoulon, D.,
Molendijk, M., Molero, P., Ortuño Sánchez-Pedreño, F., Van der Does, W., & Angel Martínez-González, M. (2018). Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. Journal of affective disorders, 226, 346–354. https://doi.org/10.1016/j.jad.2017.09.022
O’Neill, S., Minehan, M., Knight-Agarwal, C. R., & Turner, M. (2022). Depression, Is It Treatable in Adults Utilising Dietary Interventions? A Systematic Review of Randomised Controlled Trials. Nutrients, 14(7), 1398. https://doi.org/10.3390/nu14071398
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., McGuinness, L. A., … Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed.), 372, n71. https://doi.org/10.1136/bmj.n71
Pannu, A., Sharma, P. C., Thakur, V. K., & Goyal, R. K. (2021). Emerging Role of Flavonoids as the Treatment of Depression. Biomolecules, 11(12), 1825. https://doi.org/10.3390/biom11121825
Ventriglio, A., Sancassiani, F., Contu, M. P., Latorre, M., Di Slavatore, M., Fornaro, M., & Bhugra, D. (2020). Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clinical practice and epidemiology in mental health : CP & EMH, 16(Suppl-1), 156–164. https://doi.org/10.2174/1745017902016010156
Wu, P. Y., Lin, M. Y., & Tsai, P. S. (2020). Alternate healthy eating index and risk of depression: A meta-analysis and systemematic review. Nutritional neuroscience, 23(2), 101–109. https://doi.org/10.1080/1028415X.2018.1477424








Leave a comment