- A series of experiments published in Brain Behavior and Immunity revealed that exposing mice to chronic stress reduced the levels of a protein called mucin 13.
- Deleting the gene that encodes mucin 13 was sufficient to create the changes in the gut microbiome seen after exposure to chronic stress and to produce and produce depression-like symptoms.
- Mice without the gene that encodes mucin 13 were more susceptible to stress.
Depression and anxiety affect millions of people worldwide. Despite this, treatments for these disorders are often not very effective. Estimates state that at least 30% of individuals suffering from depression do not experience symptom withdrawal even after multiple treatment procedures (McIntyre et al., 2023). The situation is similar to anxiety – only about 60% of patients respond to treatments to any significant degree (Bystritsky, 2006).
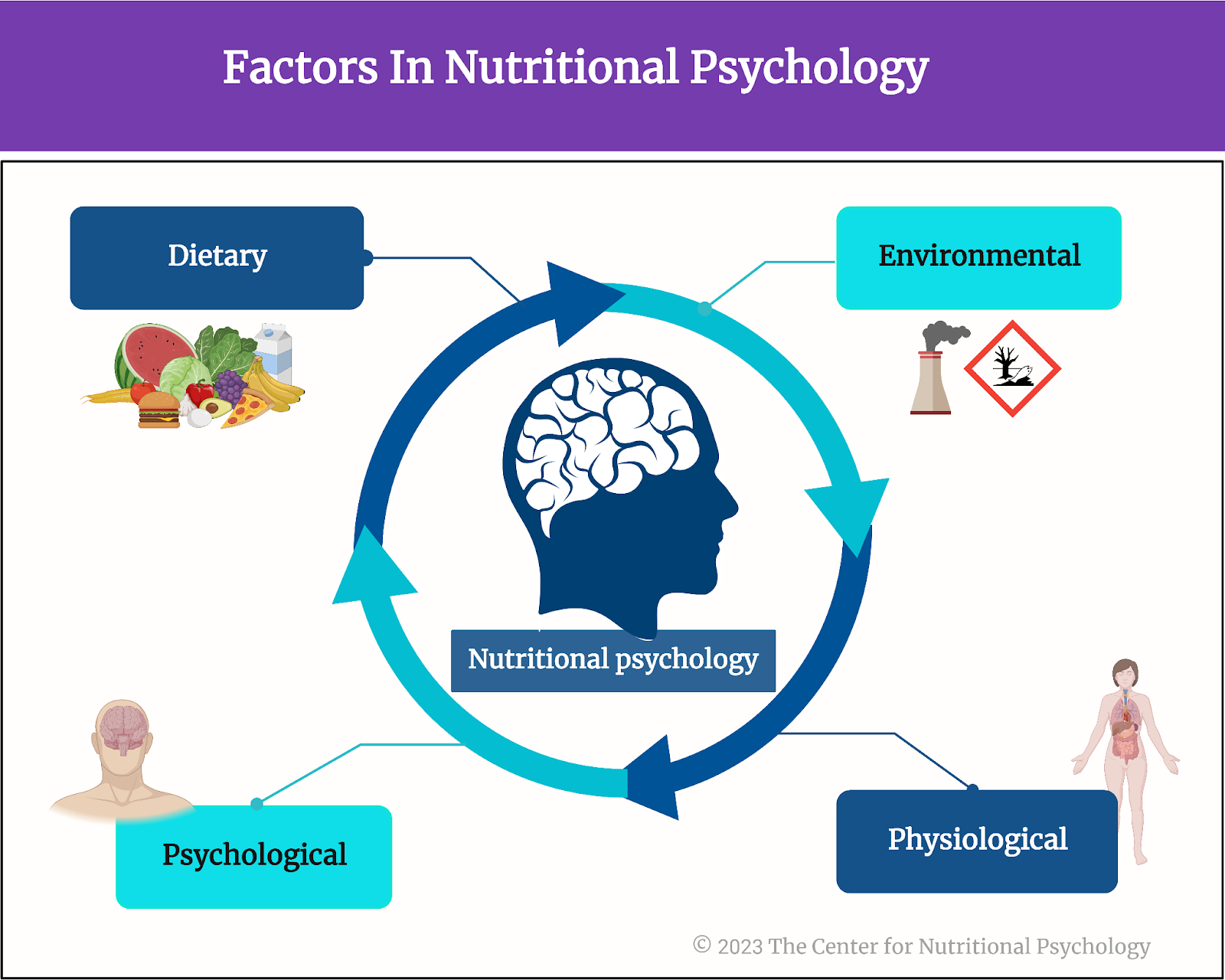
One of the reasons for the low effectiveness of treatments for these widespread disorders probably lies in the fact that their causes are not fully understood by researchers. However, the recent discovery of the microbiota-gut-brain axis (MGBA) and studies of the biochemical pathways involved in depression and anxiety show promise to change this situation (Bonaz et al., 2018; Hedrih, 2023).
The microbiota-gut-brain axis and mental health
The gut microbiota is a community of trillions of microorganisms living in our gut. These organisms help us digest the food we eat, allowing us to extract nutrients from foods that we would not be able to use without their help. However, their role in our organisms far exceeds these digestive processes.
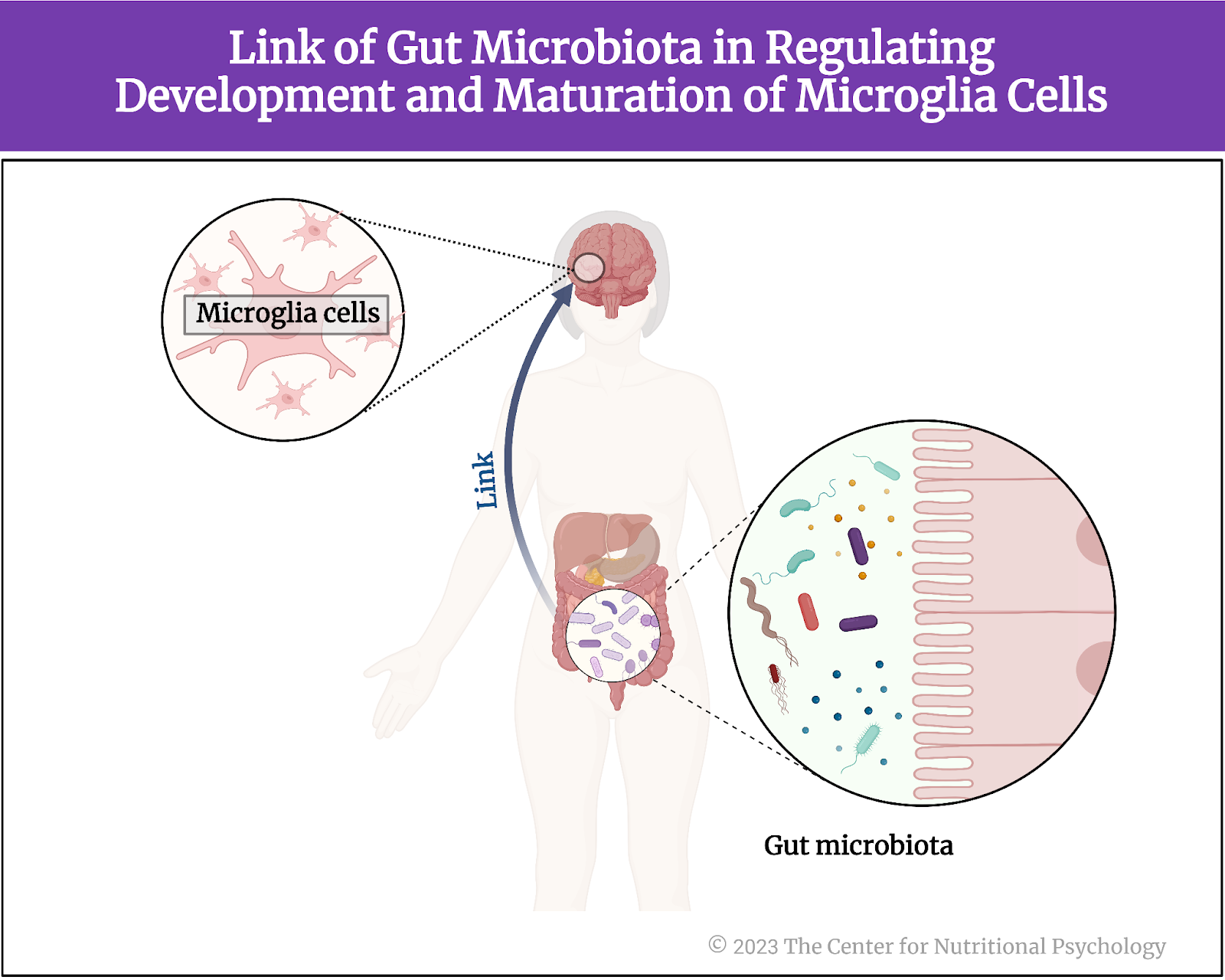
Researchers discovered a bidirectional communication pathway that allows the gut microbiota to influence processes in the brain and vice versa (Valles-Colomer et al., 2019). This pathway was named the microbiota-gut-brain axis. Studies show that individuals with specific mental health issues have altered gut microbiota composition.
Studies show that individuals with specific mental health issues have altered gut microbiota composition
Additionally, studies on rodents revealed that it is possible to transfer serious mental health symptoms, such as those of social anxiety or even cognitive deficits associated with Alzheimer’s disease, by simply transplanting gut microbiota from humans suffering from these disorders into rodents (Hedrih, 2024; Kim et al., 2021; Ritz et al., 2024). Recent studies also identified specific biochemicals regulated by gut microbiota that affect processes such as inflammation in the brain or that induce changes in the brain, resulting in behavioral alterations (Heiss et al., 2021; Ritz et al., 2024). An important finding was that exposure to chronic stress alters gut microbiota composition (Ritz et al., 2024; Rivet-Noor et al., 2024).
It is possible to transfer serious mental health symptoms by simply transplanting gut microbiota from humans suffering from these disorders into rodents
These results created hope that novel ways to treat anxiety and depression, as well as other mental health issues, might be developed after we better understand the interplay between gut microbiota and processes in the brain.
The current study
Study author Courtney R. Rivet-Noor and her colleagues noted that the mucus layer in the gut is crucial for regulating microbiome composition. This mucus layer is a protective barrier that covers the gut lining, preventing damage from digestive enzymes, pathogens, and mechanical stress. The main component of this layer is a class of proteins called mucins.
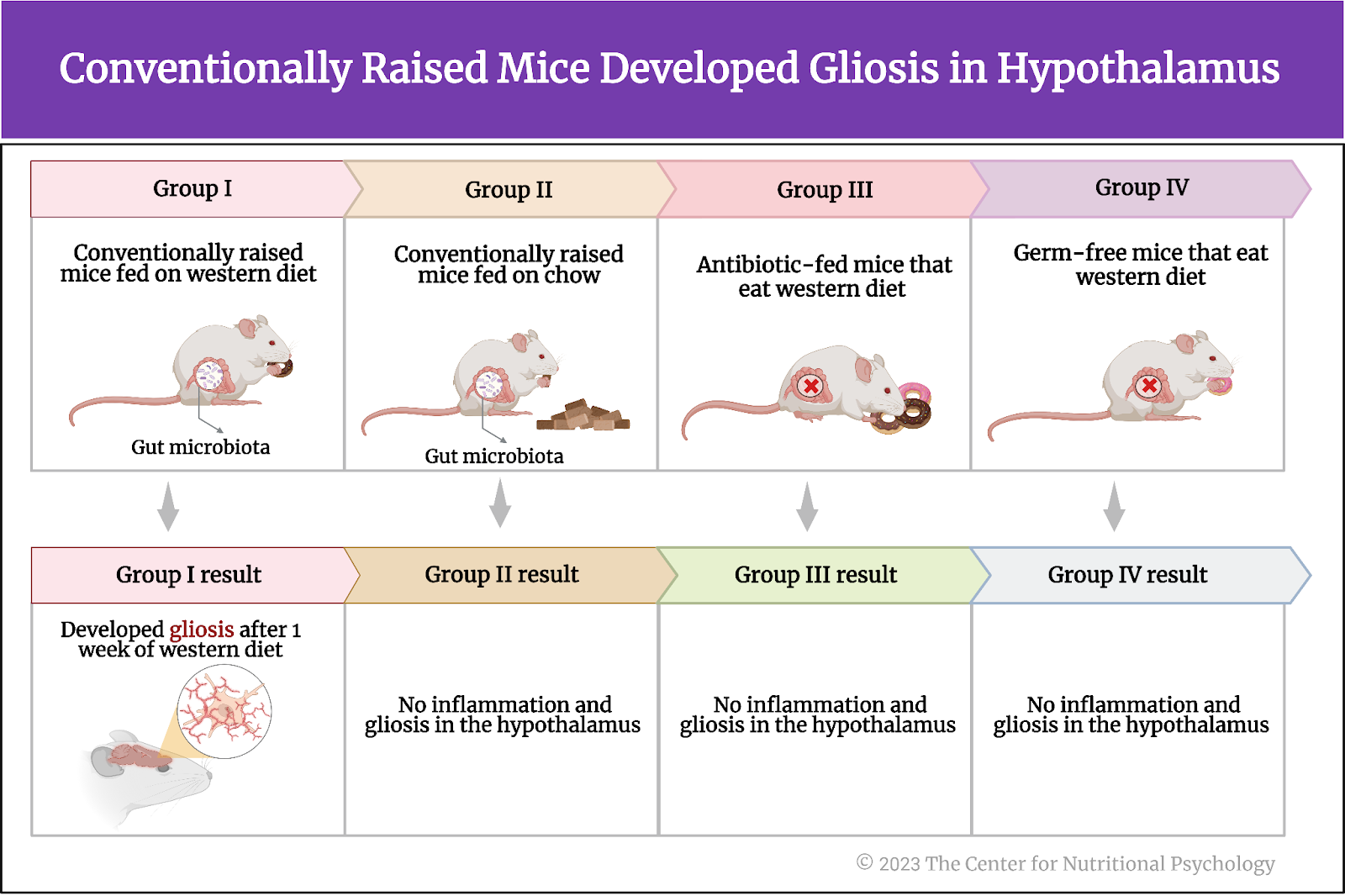
The authors of this study hypothesized that exposure to chronic stress alters this mucus layer, thus initiating microbiome changes (see Figure 1). To test this, they conducted a study on mice.

Figure 1. The mucus layer of the gut
The study procedure
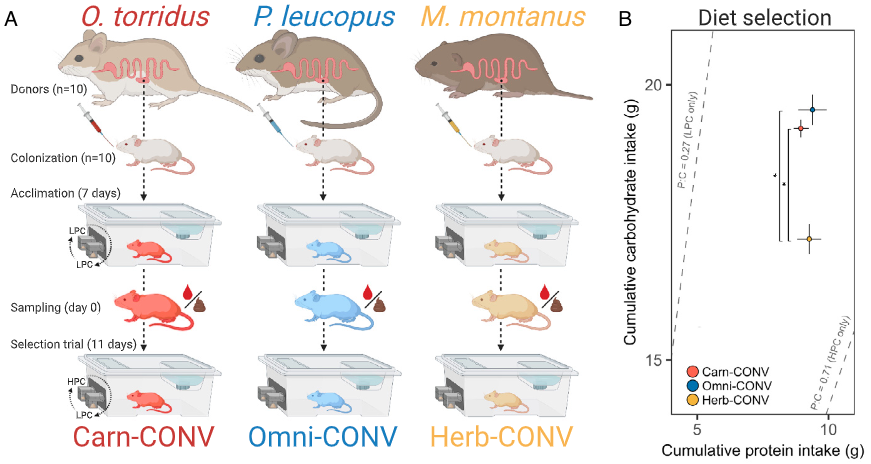
The study was conducted on two widely used strains of inbred laboratory mice (C57BL/6J and BALB/cJ). Mice were divided into two groups – one was exposed to chronic mild restraint stress by keeping them restrained in conical tubes for 2 hours and exposing them to one overnight stressor per day. The overnight stressors were 45-degree cage tilt, wet bedding, or 2x cage change. After a certain period, this treatment produces symptoms akin to depression and anxiety in humans. Mice not exposed to stress were used as controls.
The authors conducted a series of behavioral tests to test whether the stress treatment produced the expected effects (the forced swim, tail suspension, sucrose preference, open field, elevated plus maze, and nestlet shred tests). They also analyzed the tissues of these mice and conducted microbiota transfer experiments (see Figure 2).

Figure 2. Study Procedure (Rivet-Noor et al., 2024)
Chronic stress modified microbiome composition and reduced mucin 13 levels
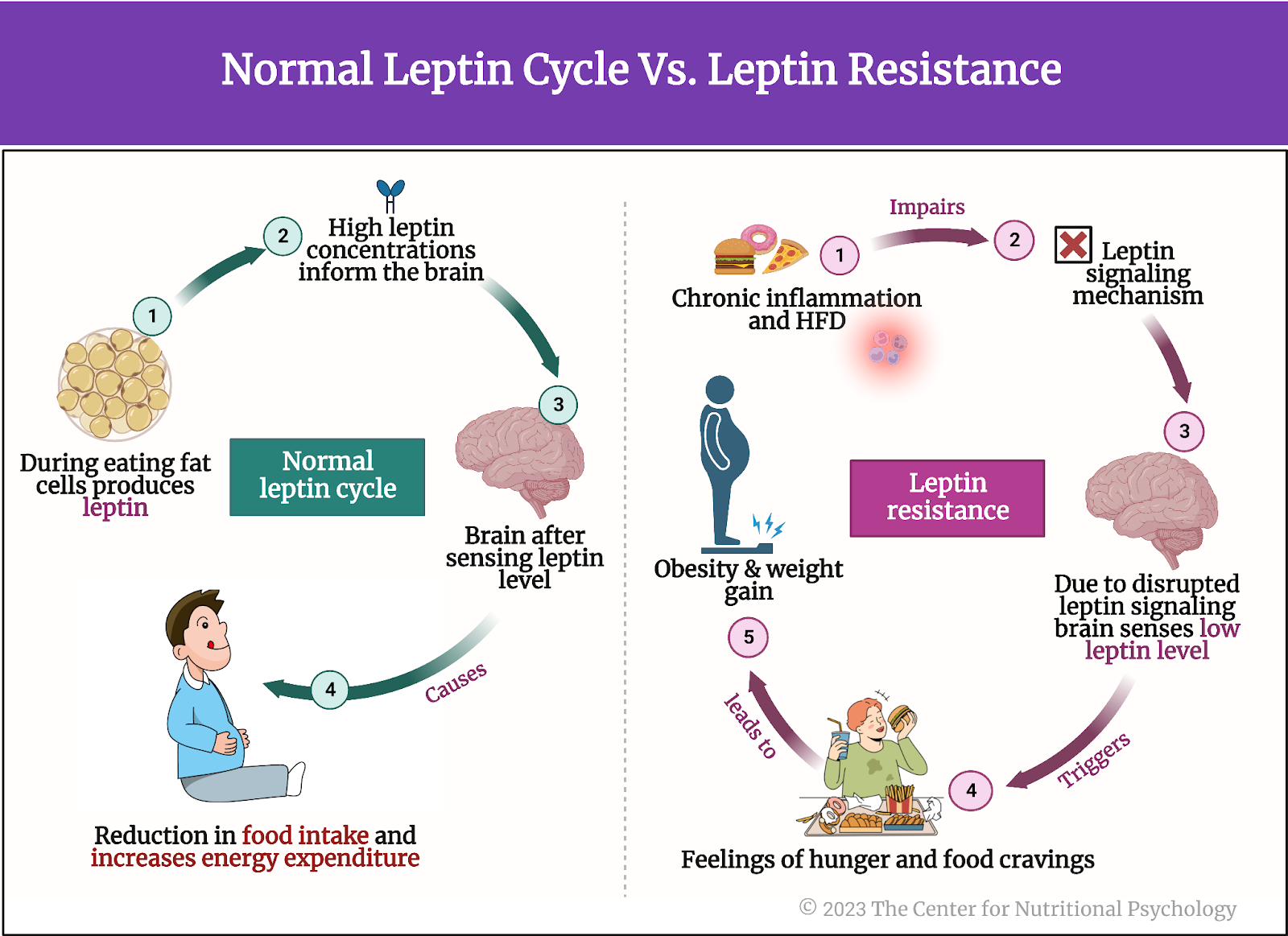
As expected, exposing mice to chronic stress increased depression and anxiety-like behaviors in exposed mice. It also altered their gut microbiota composition. These mice had reduced expression of the Muc13 gene, resulting in lower levels of one of the mucin proteins – mucin 13. Other mucin proteins were unaffected.
Transferring gut microbiota from stressed mice to mice not exposed to chronic stress did not affect mucin 13 levels in the recipient mice. However, transplanting gut microbiota from stressed mice into mice without gut microbiota made the latter group of mice develop depression and anxiety-like symptoms, although they were not exposed to stress. This meant that mucin 13 reductions were not driven by changes in gut microbiota, but gut microbiota changes did lead to depression- and anxiety-like symptoms (see Figure 3).

Figure 3. Chronic stress modified microbiome composition and reduced mucin 13 levels
Deleting the Muc13 gene leads to microbiome changes similar to those resulting from chronic stress
The reduction in the expression of the Muc13 gene was caused by a protein called hepatocyte nuclear factor 4 or HNF4. This protein regulates the expression of specific genes by binding to particular DNA sequences. Analysis showed that chronic stress reduced the production of HNF4, leading to lower expression of the Muc13 gene. This was independent of changes to the microbiome.
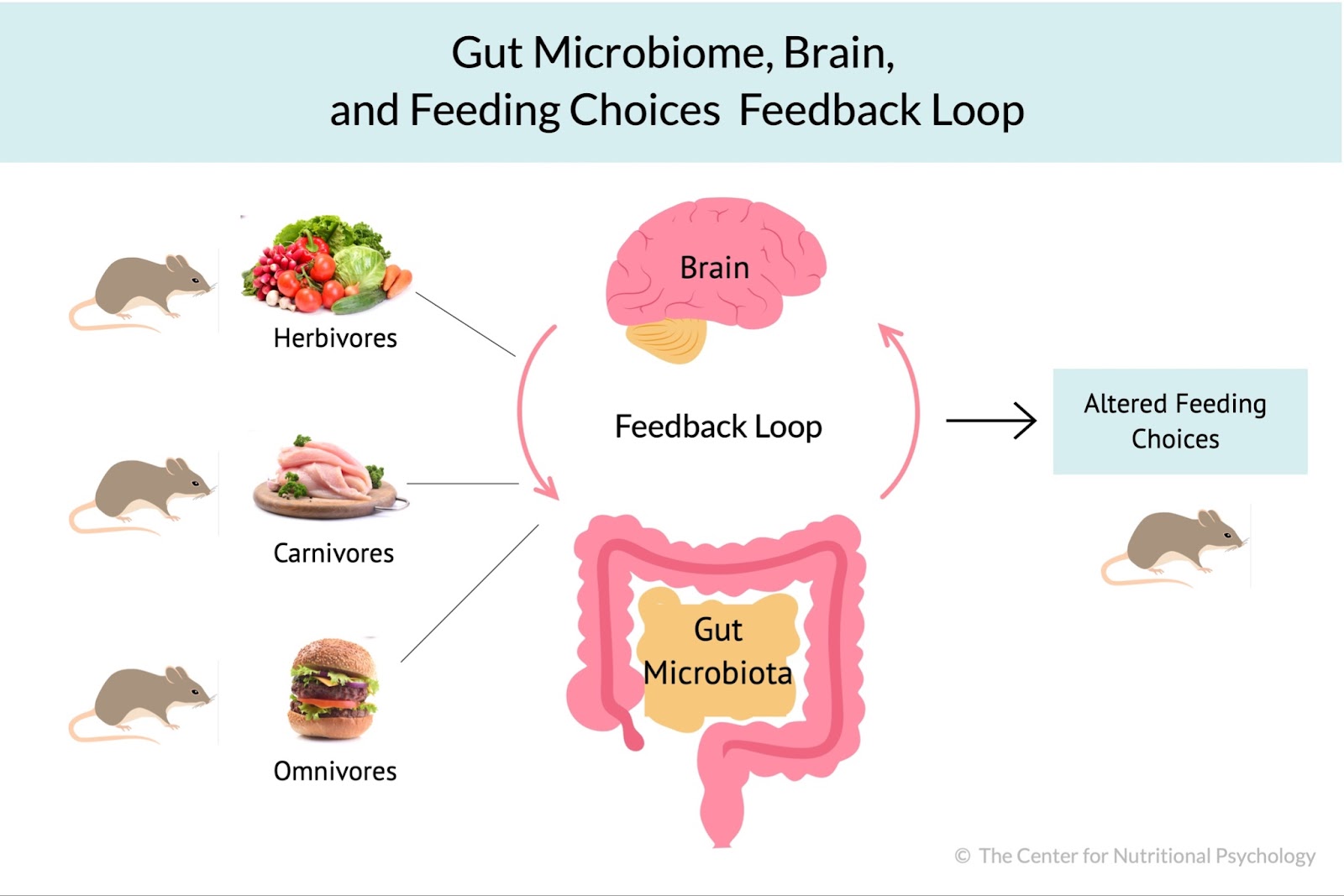
Finally, the study authors created a line of mice without the Muc13 gene. Without being exposed to chronic stress, these mice had microbiota composition resembling regular mice exposed to chronic stress. This suggested that reductions in mucin 13 protein drive the changes in microbiota after experiencing chronic stress.
Behavioral tests showed that mice without the Muc13 gene displayed depression-like but not anxiety-like behaviors without being exposed to stress. However, after being exposed to stress, mice without the Muc13 gene developed anxiety-like symptoms much faster (after only one week) than regular mice. This indicated that the lack of this gene and the consequent lack of mucin 13 made them more susceptible to the effects of stress (see Figure 4).

Figure 4. Effects of absence of Muc13 gene in Mice
Conclusion
The study showed that chronic stress’s effects on behavior are mediated by a protein in the mucus layer of the gut called mucin 13. Although the study was done on mice, mucin 13 also exists in the human gut. This discovery could potentially open new ways to treat the consequences of chronic stress by targeting the production or level of mucin 13 in the gut.
The paper “Stress-induced mucin 13 reductions drive intestinal microbiome shifts and despair behaviors” was authored by Courtney R. Rivet-Noor, Andrea R. Merchak, Caroline Render, Naudia M. Gay, Rebecca M. Beiter, Ryan M. Brown, Austin Keeler, G. Brett Moreau, Sihan Li, Deniz G. Olgun, Alexandra D. Steigmeyer, Rachel Ofer, Tobey Phan, Kiranmayi Vemuri, Lei Chen, Keira E. Mahoney, Jung-Bum Shin, Stacy A. Malaker, Chris Deppmann, Michael P. Verzi, and Alban Gaultier.
References
Bonaz, B., Bazin, T., & Pellissier, S. (2018). The vagus nerve at the interface of the microbiota-gut-brain axis. Frontiers in Neuroscience, 12(FEB). https://doi.org/10.3389/fnins.2018.00049
Bystritsky, A. (2006). Treatment-resistant anxiety disorders. Molecular Psychiatry, 11(9), 805–814. https://doi.org/10.1038/sj.mp.4001852
Hedrih, V. (2023, September 2). Gut Microbiota’s Role in Mental Health: The Positives and Negatives. CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/how-your-gut-microbiota-is-linked-to-both-positive-and-negative-aspects-of-mental-health/
Hedrih, V. (2024, March 12). Can Social Anxiety From Humans be Transmitted to Mice? CNP Articles in Nutritional Psychology. https://www.nutritional-psychology.org/can-social-anxiety-from-humans-be-transmitted-to-mice/
Heiss, C. N., Mannerås-Holm, L., Lee, Y. S., Serrano-Lobo, J., Håkansson Gladh, A., Seeley, R. J., Drucker, D. J., Bäckhed, F., & Olofsson, L. E. (2021). The gut microbiota regulates hypothalamic inflammation and leptin sensitivity in Western diet-fed mice via a GLP-1R-dependent mechanism. Cell Reports, 35(8). https://doi.org/10.1016/j.celrep.2021.109163
Kim, N., Jeon, S. H., Ju, I. G., Gee, M. S., Do, J., Oh, M. S., & Lee, J. K. (2021). Transplantation of gut microbiota derived from Alzheimer’s disease mouse model impairs memory function and neurogenesis in C57BL/6 mice. Brain, Behavior, and Immunity, 98, 357–365. https://doi.org/10.1016/J.BBI.2021.09.002
McIntyre, R. S., Alsuwaidan, M., Baune, B. T., Berk, M., Demyttenaere, K., Goldberg, J. F., Gorwood, P., Ho, R., Kasper, S., Kennedy, S. H., Ly-Uson, J., Mansur, R. B., McAllister-Williams, R. H., Murrough, J. W., Nemeroff, C. B., Nierenberg, A. A., Rosenblat, J. D., Sanacora, G., Schatzberg, A. F., … Maj, M. (2023). Treatment-resistant depression: Definition, prevalence, detection, management, and investigational interventions. World Psychiatry, 22(3), 394–412. https://doi.org/10.1002/wps.21120
Ritz, N. L., Brocka, M., Butler, M. I., Cowan, C. S. M., Barrera-Bugueño, C., Turkington, C. J. R., Draper, L. A., Bastiaanssen, T. F. S., Turpin, V., Morales, L., Campos, D., Gheorghe, C. E., Ratsika, A., Sharma, V., Golubeva, A. V., Aburto, M. R., Shkoporov, A. N., Moloney, G. M., Hill, C., … Cryan, J. F. (2024). Social anxiety disorder-associated gut microbiota increases social fear. Proceedings of the National Academy of Sciences, 121(1), e2308706120. https://doi.org/10.1073/pnas.2308706120
Rivet-Noor, C. R., Merchak, A. R., Render, C., Gay, N. M., Beiter, R. M., Brown, R. M., Keeler, A., Moreau, G. B., Li, S., Olgun, D. G., Steigmeyer, A. D., Ofer, R., Phan, T., Vemuri, K., Chen, L., Mahoney, K. E., Shin, J.-B., Malaker, S. A., Deppmann, C., … Gaultier, A. (2024). Stress-induced mucin 13 reductions drive intestinal microbiome shifts and despair behaviors. Brain, Behavior, and Immunity, 119, 665–680. https://doi.org/10.1016/j.bbi.2024.03.028
Valles-Colomer, M., Falony, G., Darzi, Y., Tigchelaar, E. F., Wang, J., Tito, R. Y., Schiweck, C., Kurilshikov, A., Joossens, M., Wijmenga, C., Claes, S., Van Oudenhove, L., Zhernakova, A., Vieira-Silva, S., & Raes, J. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology, 4(4), 623–632. https://doi.org/10.1038/s41564-018-0337-x