Mental Health Professionals Report Poor Literacy for Nutritional Medicine: International Survey

Evidence supports the use of nutritional interventions for certain psychiatric symptoms, yet few studies have evaluated nutritional literacy among mental health professionals (MHPs). One such study is the online survey published by Mörkl et al. (2021), which gathered data from a sample of mental health professionals from 52 countries.
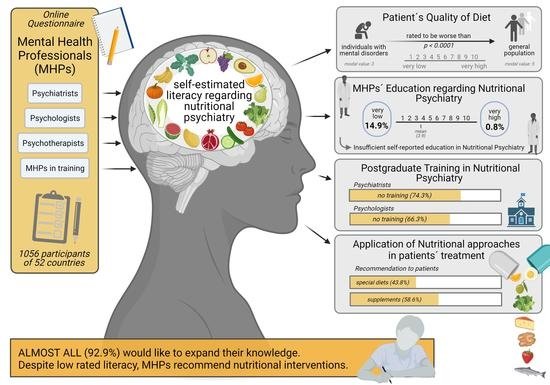
The survey collected data about general nutrition knowledge, nutrition education, learning opportunities, and the tendency to recommend or prescribe food supplements and diets. The sample included psychologists, psychiatrists, psychotherapists and MHPs in-training. Most participants were from Europe but the sample also included professionals from Asia, North America, Oceania, South America, and Africa.
The majority of the participants (92.9%) wanted to expand their knowledge of Nutritional Psychiatry and only 0.8% of them rated their nutrition education as ‘very good’. In fact, most of the participants had no training in nutrition yet many did use nutrition approaches with their patients, with as many as 58.6% of them recommending supplements and 43.8% recommending diet strategies to their patients. Nutritional approaches to treatment were most often used for treating eating and affective disorders, followed by anxiety, psychotic, and obsessive-compulsive disorders.
While most mental health professionals in the survey did not have any training in nutrition, the beliefs about nutrition reported by most of them align with what the data says. For instance, most believed that mental disorders are associated with poor nutrition and evidence shows that individuals with mental health problems often have an unhealthy lifestyle, including poor dietary choices, disordered eating behaviors, and nutritional deficiencies (Teasdale et al., 2019; Gill, 2021). Furthermore, the professionals interviewed often used nutritional approaches for affective disorders, a practice that is supported by research, including a meta-analysis of 16 randomized controlled trials which found that nutritional interventions significantly reduced symptoms of depression, especially when the interventions were provided by accredited nutritional professionals (Firth et al., 2019).
The authors of the survey hypothesized that psychiatrists may have a tendency to overrate their understanding of nutrition compared to other mental health professionals due to their medical training. This may imply that some of them may provide misguided nutrition advice due to lack of training. It is worth noticing that, in the US, for example, only 40% of medical schools reach the goal of teaching 25 h of nutrition in preclinical years (Adams, Lindell, Kohlmeier & Zeisel, 2006).
Two main points can be made out of the results of this survey. First, many mental health professionals do not use nutritional interventions, either because they are not aware of the relevance of such interventions or because they do not have the training to do it. Second, while most mental health experts do use nutritional approaches to treatment, many may lack the knowledge necessary to provide adequate nutritional counselling. Introducing nutrition education in the educational curricula of mental health professionals may improve the quality of mental health services and, consequently, of mental health outcomes.
References
Adams, K. M., Lindell, K. C., Kohlmeier, M., & Zeisel, S. H. (2006). Status of nutrition education in medical schools. The American Journal of Clinical Nutrition, 83(4), 941S-944S.
Gill, R., Tyndall, S. F., Vora, D., Hasan, R., Megna, J. L., & Leontieva, L. (2021). Diet Quality and Mental Health Amongst Acute Inpatient Psychiatric Patients. Cureus, 13(1), e12434. https://doi.org/10.7759/cureus.12434
Firth, J., Marx, W., Dash, S., Carney, R., Teasdale, S. B., Solmi, M., … & Sarris, J. (2019). The effects of dietary improvement on symptoms of depression and anxiety: a meta-analysis of randomized controlled trials. Psychosomatic Medicine, 81(3), 265.
Mörkl, S., Stell, L., Buhai, D. V., Schweinzer, M., Wagner-Skacel, J., Vajda, C., … & Holasek, S. J. (2021). ‘An Apple a Day’?: Psychiatrists, Psychologists and Psychotherapists Report Poor Literacy for Nutritional Medicine: International Survey Spanning 52 Countries. Nutrients, 13(3), 822. https://www.mdpi.com/2072-6643/13/3/822
Teasdale, S. B., Ward, P. B., Samaras, K., Firth, J., Stubbs, B., Tripodi, E., & Burrows, T. L. (2019). Dietary intake of people with severe mental illness: systematic review and meta-analysis. The British Journal of Psychiatry, 214(5), 251-259.








Leave a comment