The bidirectional relationship between the gut microbiome and mental health: a comprehensive review

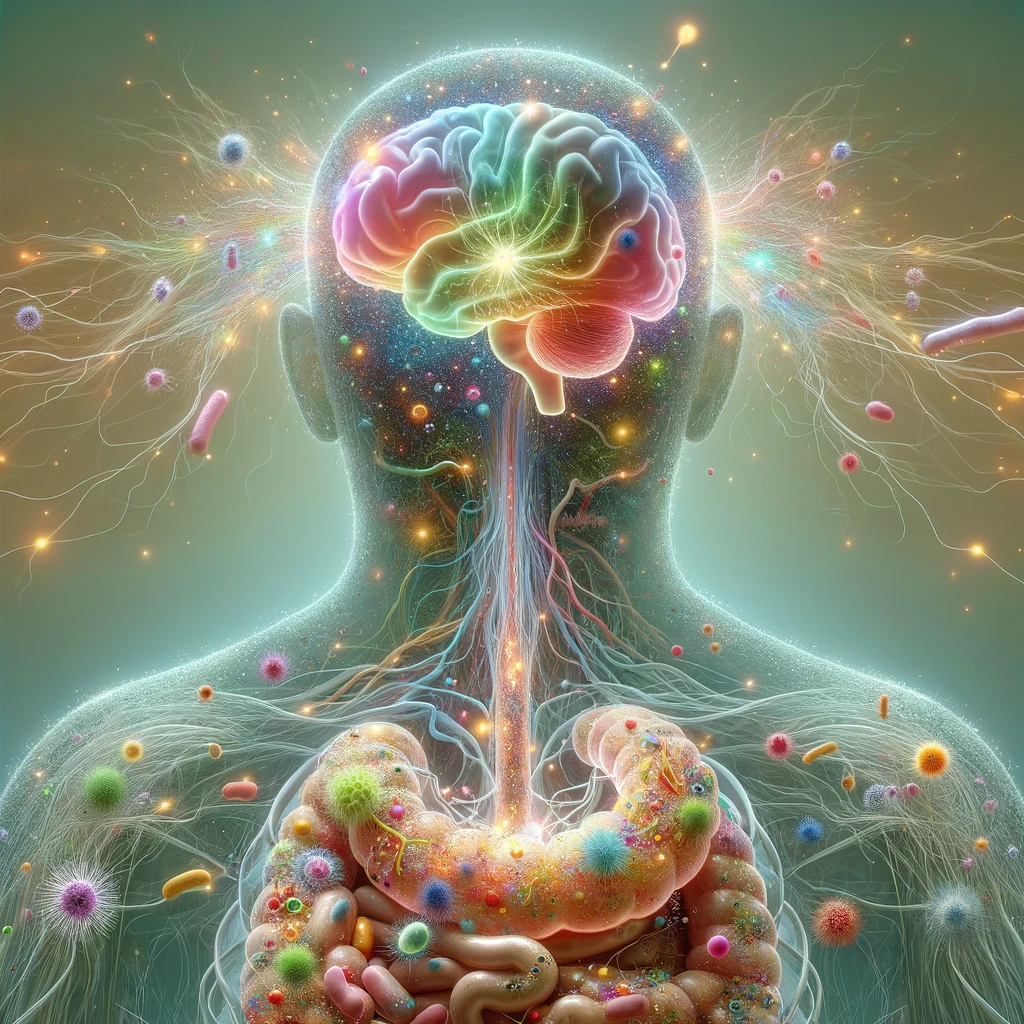
The gut microbiome plays a crucial role in mental well-being by affecting mood, cognition, and emotional regulation via the gut-brain axis. This two-way communication system links the gastrointestinal and central nervous systems through microbial metabolites, neurotransmitters, and immune system interactions. According to recent research, mental health issues, including anxiety, sadness, and stress-related ailments, are linked to dysbiosis, or disturbances in the equilibrium of gut microbes. Altered gut diversity, reduced short-chain fatty acids (SCFAs) production, and increased neuroinflammation are key contributors to these disturbances. This article by Rathore et al. (2025) examines how the gut microbiome influences brain function through mechanisms such as microbial neurotransmitter production, vagus nerve activity, and modulation of the hypothalamic-pituitary-adrenal (HPA) axis. It also reviews microbiome-targeted therapies—including probiotics, prebiotics, dietary changes, and fecal microbiota transplantation (FMT) for their potential to ease psychiatric symptoms. Personalized microbiome-based therapies are becoming possible because of developments in bioinformatics and microbiome sequencing. However, challenges such as individual variability, inconsistent methods, and the need for long-term studies persist. Future directions include standardizing assessment tools and integrating microbiome science into precision psychiatry to revolutionize mental health care. [NPID: Dysbiosis, gut-brain axis, gut microbiome, mental health, neuroinflammation, probiotics, short-chain fatty acids]
Year: 2025
 Navigation
Navigation