Study Finds Daily Changes in Gut Microbiota Influence Our Stress Response

Listen to this Article
- A study on mice published in Cell Metabolism found that daily oscillations in gut microbiota composition regulate natural daily patterns of corticosterone release.
- Depletion of gut microbiota results in impairments in stress responsivity that are specific to certain times of day and in disruptions in the rhythmicity of stress pathways in the brain.
- In this way, gut microbiota regulate the body’s responsivity to stress.
We have all experienced situations that upset us. There are situations where we feel threatened or are afraid of something, or situations that require us to exert ourselves to prevent undesirable things from happening to us. Most often, we noticed our heart starting to beat faster, and a whole range of changes in our bodies became noticeable. In such situations, we experience stress.
Stress
Stress is the body’s natural response to a perceived threat or challenge. Physiologically, it activates the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis (also known as the HPA axis), triggering the “fight-or-flight” response. The hypothalamus releases corticotropin-releasing hormone, which stimulates the pituitary gland to secrete adrenocorticotropic hormone, leading the adrenal cortex to release cortisol, the main stress hormone. At the same time, the adrenal medulla releases adrenaline. Adrenaline and cortisol increase heart rate, blood pressure, and glucose availability for quick energy. Breathing becomes faster, muscles tense, and digestion slows to redirect resources toward immediate survival (Chrousos, 2000; Herman et al., 2016; Russell & Lightman, 2019).
Once the stressor passes, the parasympathetic nervous system helps restore balance and normal function. Chronic activation of this stress response can harm the immune system, cardiovascular health, and overall well-being.
Acute and chronic stress
The process described above refers to acute stress. However, stress can also be chronic. While acute stress is the body’s immediate reaction to a sudden challenge or threat, chronic stress occurs when stressors (situations that cause the stress reaction) persist over a long period. For example, such stressors could include ongoing financial worries, relationship difficulties, demanding jobs, or life in a war zone.
Prolonged activation of the stress response keeps cortisol levels elevated, which can suppress immunity, disrupt sleep, increase risk of depression, eating disorders, and other mental health disorders, make the body more responsive to future acute stress, create adverse changes in the brain affecting memory, contribute to cardiovascular and metabolic diseases, and is associated with a wide range of other adverse health outcomes (Adell et al., 1988; Dallman et al., 2005; Gouin, 2011, 2011; Khan et al., 2020; Torpy et al., 2007).
The current study
Study author Gabriel S.S. Tofani and his colleagues note that systems in our body regulating stress are intertwined with those regulating circadian rhythms (Tofani et al., 2025). They consider this an evolutionary adaptation that enables the organism to adapt to environmental changes. Circadian rhythm is the body’s internal 24-hour biological clock that regulates cycles of sleep, wakefulness, hormone release, and other physiological processes in response to light and darkness.
Through evolution, there were times of day when dangerous and challenging situations were the most likely to occur and times of day when they were less likely. Before the invention of electric lighting, humans were primarily active during daylight hours, with most activities occurring in the morning. As a result, our bodies have adapted to being most responsive to stress at that time. The levels of the stress hormone cortisol peak in the morning (this is called the cortisol awakening response), and tend to decline in the evening, when the light fades (Steptoe & Serwinski, 2016).
The authors of this study investigated the role of the gut microbiota, the community of microorganisms residing in the gut, in the interplay between circadian rhythms and stress responsivity. More specifically, they aimed to investigate how this interplay operates when gut microbiota are removed from the gut.
The authors investigated the role of the gut microbiota in the interplay between circadian rhythms and stress responsivity.
The study was conducted on 7–14-week-old C57BL/6 mice, an inbred strain of laboratory mice widely used in research due to their genetic uniformity and well-established physiological characteristics.
Some of these mice were given drinking water containing a cocktail of antibiotics: ampicillin sodium salt (1 g/L), gentamicin sulfate (1 g/L), vancomycin hydrochloride (0.5 g/L), and imipenem (0.25 g/L) for 14 days. The goal of this treatment was to eliminate their gut microbiota. After this was achieved, some of the mice received a transfer of gut microbiota from feces in the form of two injections 72 hours apart. This resulted in the treated mice acquiring a new gut microbiota. Some other mice received a probiotic – Limosilactobacillus reuteri bacterium, allowing researchers to see whether this would reverse the effects of gut microbiota depletion on stress-related physiological parameters.
Some mice were controls and did not undergo treatments. After the treatments, the mice were exposed to a situation that induces stress (immobilization), and the study authors examined their behavioral reactions and physiological parameters, as well as tissues (see Figure 1).
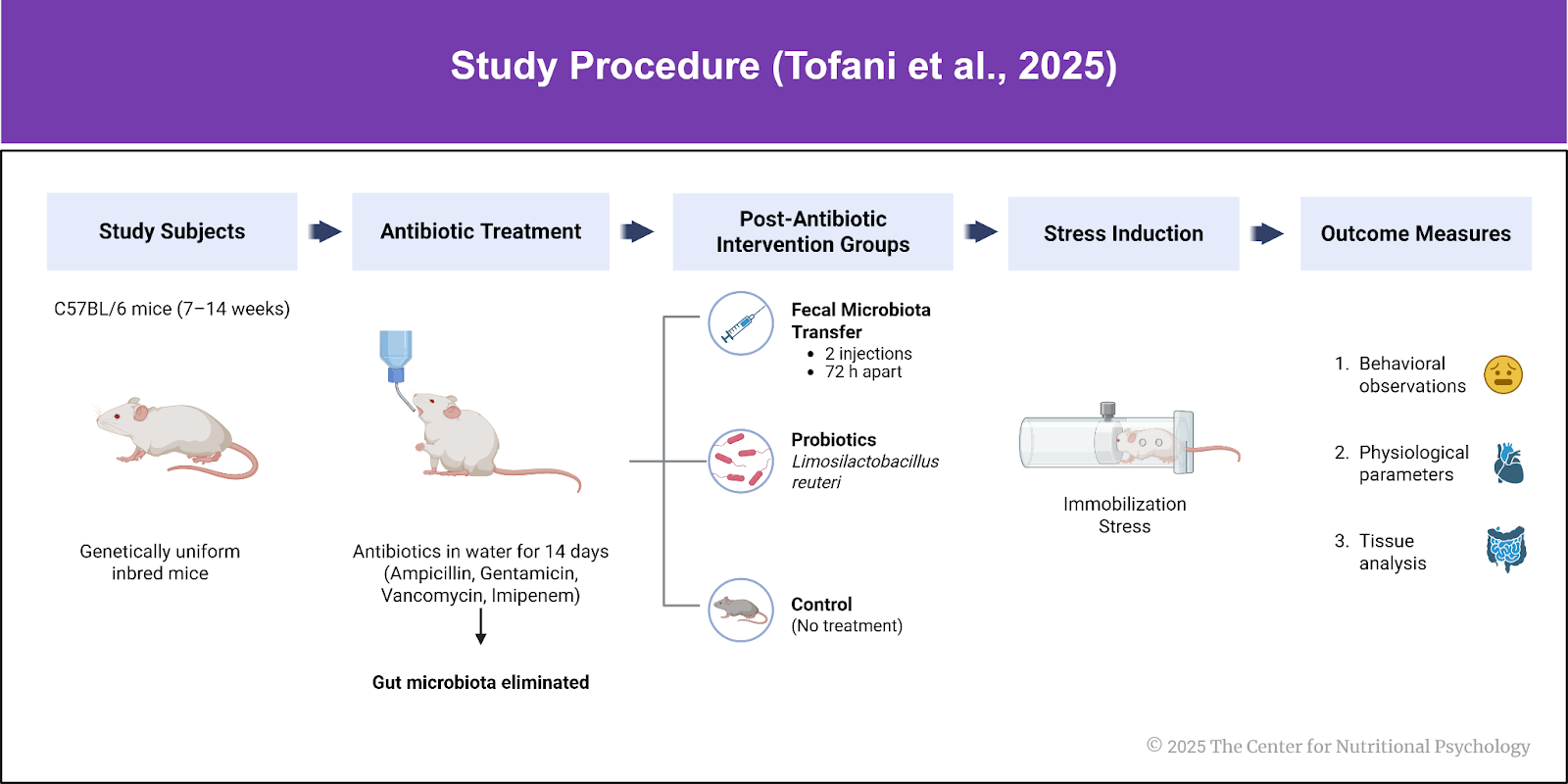
Figure 1. Study procedure (Tofani et al., 2025)
Gut microbiota composition oscillates across the day and modulates rhythms of corticosterone
Results showed that gut microbiota composition oscillates across the day and modulates the daily rhythm of change in corticosterone levels. Corticosterone is a hormone in mice that plays the same role as cortisol in humans. In mice with destroyed gut microbiota, the rhythm of corticosterone change was disrupted. A detailed analysis (RNA sequencing) revealed that the absence of gut microbiota affected the structure of the brain, specifically the suprachiasmatic nucleus (SCN), which is crucial for maintaining circadian rhythms.
The absence of gut microbiota affected the structure of the brain that is central for maintaining the circadian rhythms, called the suprachiasmatic nucleus
In mice with destroyed gut microbiota, the functioning of the HPA axis, and thus stress responsiveness, was also disrupted. Their reactions to stress, social interaction, and anxiety-like behaviors were changed, and this depended on the time of day. The blood-brain barrier in the hypothalamus was also impaired in these mice. Restoring gut microbiota through fecal microbiota transfer and administering the probiotic bacterium Limosilactobacillus reuteri normalized certain aspects of stress reactivity (see Figure 2).
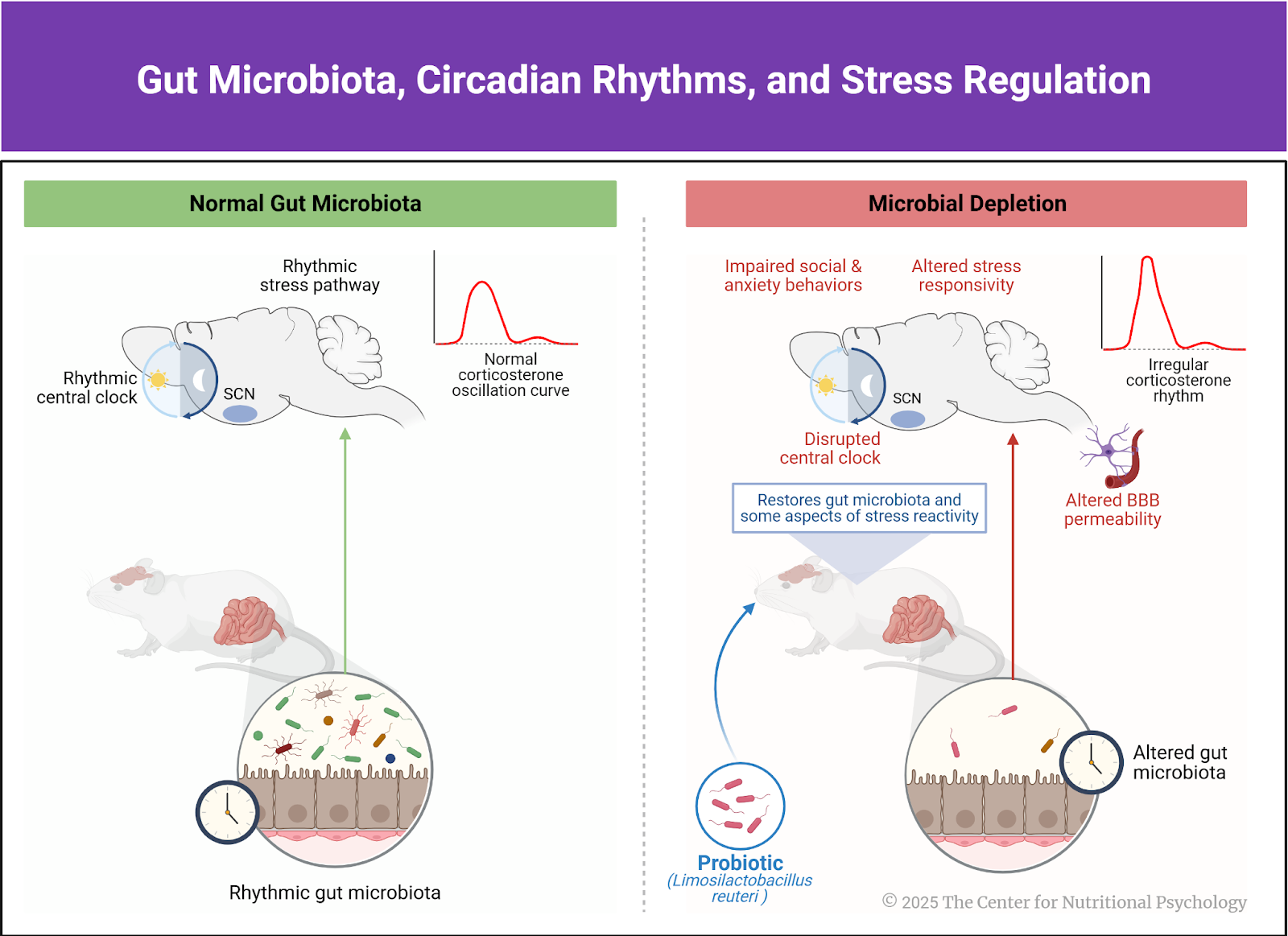
Figure 2. Gut microbiota, Circadian rhythm, and stress regulation
In mice with destroyed gut microbiota, the functioning of the HPA axis, and thus stress responsiveness, was also disrupted.
Conclusions
The study revealed that gut microbiota composition fluctuates throughout the day and regulates the activity of brain areas responsible for circadian rhythms and stress responses. In this way, gut microbiota regulate the daily rhythms of the body’s system responsible for stress.
Although the study was conducted on mice and not humans, humans and mice share many physiological similarities, so it is reasonably expected that the findings in humans would not differ significantly from those in mice. This potentially opens ways through which individual responsivity to stress could be affected by using probiotics and other ways to modulate gut microbiota composition.
The paper “Gut microbiota regulates stress responsivity via the circadian system” was authored by Gabriel S.S. Tofani, Sarah-Jane Leigh, Cassandra E. Gheorghe, Paromita Sen, Gerard Clarke, and John F. Cryan.
To learn more about the microbiota-gut-brain axis and mental health, visit the Nutritional Psychology Research Library, the world’s largest online library of research connecting nutrition and mental health, or take our evidence-based continuing education courses for professionals. Visit www.nutritional-psychology.org. CNP is a non-profit educational organization building the way to a healthier future. Join us!
References
Adell, A., Garcia-Marquez, C., Armario, A., & Gelpi, E. (1988). Chronic Stress Increases Serotonin and Noradrenaline in Rat Brain and Sensitizes Their Responses to a Further Acute Stress. Journal of Neurochemistry, 50(6), 1678–1681. https://doi.org/10.1111/j.1471-4159.1988.tb02462.x
Chrousos, G. P. (2000). The Hpa Axis and the Stress Response. Endocrine Research, 26(4), 513–514. https://doi.org/10.3109/07435800009048562
Dallman, M. F., Pecoraro, N. C., & La Fleur, S. E. (2005). Chronic stress and comfort foods: Self-medication and abdominal obesity. Brain, Behavior, and Immunity, 19(4), 275–280. https://doi.org/10.1016/J.BBI.2004.11.004
Gouin, J.-P. (2011). Chronic Stress, Immune Dysregulation, and Health. American Journal of Lifestyle Medicine, 5(6), 476–485. https://doi.org/10.1177/1559827610395467
Herman, J. P., McKlveen, J. M., Ghosal, S., Kopp, B., Wulsin, A., Makinson, R., Scheimann, J., & Myers, B. (2016). Regulation of the hypothalamic-pituitary-adrenocortical stress response. Comprehensive Physiology, 6(2), 603–621. https://doi.org/10.1002/cphy.c150015
Khan, A. R., Geiger, L., Wiborg, O., & Czéh, B. (2020). Stress-Induced Morphological, Cellular and Molecular Changes in the Brain—Lessons Learned from the Chronic Mild Stress Model of Depression. Cells, 9(4), 1026. https://doi.org/10.3390/cells9041026
Russell, G., & Lightman, S. (2019). The human stress response. Nature Reviews Endocrinology, 15(9), 525–534. https://doi.org/10.1038/s41574-019-0228-0
Steptoe, A., & Serwinski, B. (2016). Chapter 34—Cortisol Awakening Response. In G. Fink (Ed.), Stress: Concepts, Cognition, Emotion, and Behavior (pp. 277–283). Academic Press. https://doi.org/10.1016/B978-0-12-800951-2.00034-0
Tofani, G. S. S., Leigh, S.-J., Gheorghe, C. E., Bastiaanssen, T. F. S., Wilmes, L., Sen, P., Clarke, G., & Cryan, J. F. (2025). Gut microbiota regulates stress responsivity via the circadian system. Cell Metabolism, 37(1), 138-153.e5. https://doi.org/10.1016/j.cmet.2024.10.003
Torpy, J. M., Lynm, C., & Glass, R. M. (2007). Chronic Stress and the Heart. JAMA, 298(14), 1722. https://doi.org/10.1001/jama.298.14.1722
 Navigation
Navigation










Leave a comment