Infant saliva microbiome activity modulates nutritional impacts on neurodevelopment
CNP Research Summary can be found in the CNP Library Membership
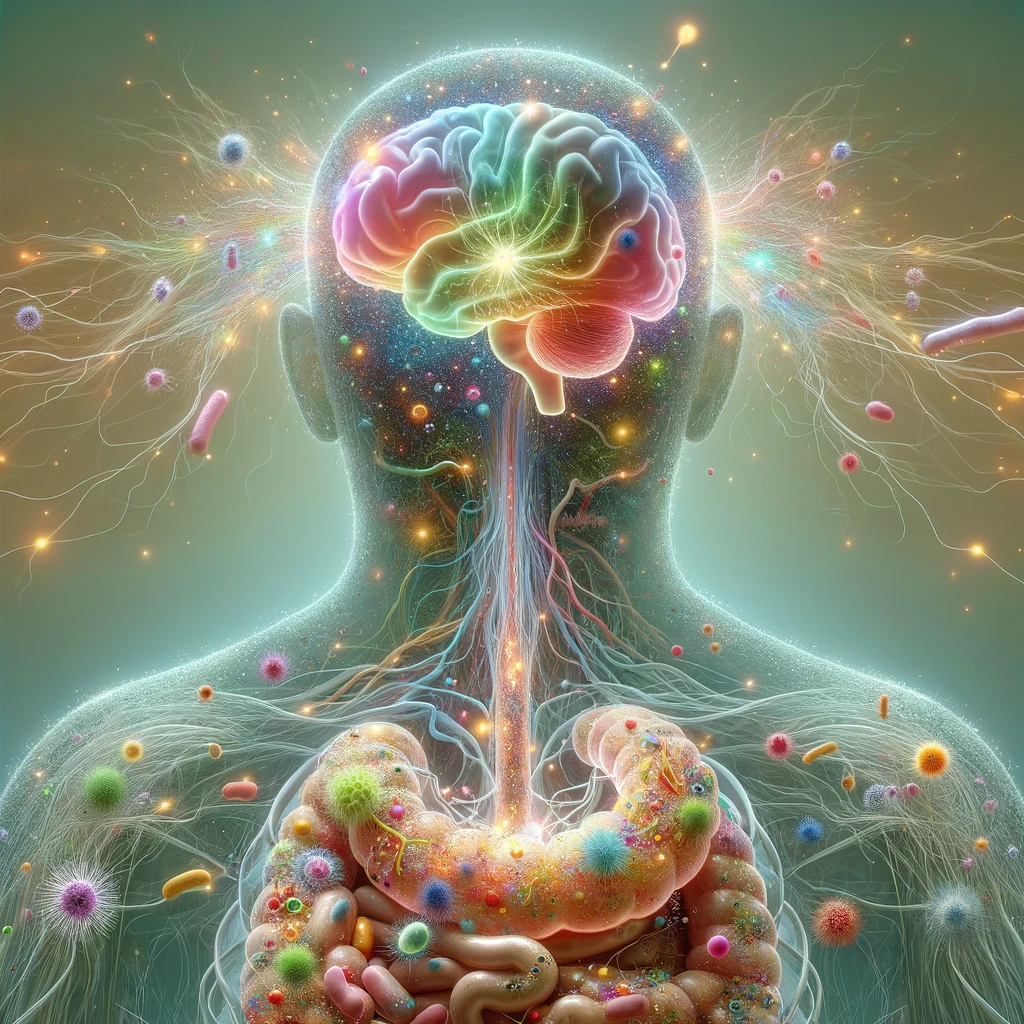

The CNP Microbiota-Gut-Brain Axis (MGBA) & Mental Health Research Category consolidates research exploring the interconnected relationship between dietary intake, the microbiome, and the gut-brain axis in the adult population. To view each original study on the open internet, click “Original.” To view the CNP-written abstract summary, click “CNP Summary.” While only some of the CNP-written abstract summaries are available below for free, all abstract summaries are available to CNP members through the CNP Library Membership.

Major depressive disorder (MDD), being a complicated condition in nature, affects 280 million individuals globally and is a primary cause of disability. Numerous environmental variables, including medicines, nutrition, and microorganisms, have a role in the pathophysiology of depression disorders. The host immune system, genetics, and epigenetics are some of the contributors to the intricate underlying causes of depression. Alterations to intestinal microbiota and their metabolites affect how people with depressive disorders respond to stress and behave in social situations by influencing immune cell maturation and brain neurogenesis, which is mediated by epigenetic changes. In this study, Nohesara et al. (2023) address the possible contributions of dysregulated gut permeability to the emergence of depressive illnesses through changes in metabolites generated from the gut microbiota that have epigenetic consequences. In addition, the authors discuss how changes in the makeup of the gut microbiota might lead to epigenetic changes that can cause depressive illnesses. Focus is shed on the potential benefits of microbiota-derived metabolites, such as probiotics, butyrate (which acts as an epigenetic modifier), polyphenols, medications (such as antibiotics, antipsychotics, and antidepressants), maternal diet, and fecal microbiota transplantation, in mitigating depressive-like behaviors through altering the epigenetic landscape. Lastly, the authors review the difficulties and potential solutions connected to current treatment techniques for depressive disorders via microbiome-related epigenetic changes.
Infant saliva microbiome activity modulates nutritional impacts on neurodevelopment
CNP Research Summary can be found in the CNP Library Membership
Exploring the effects of a Mediterranean Diet and weight loss on the gut microbiome and cognitive performance in older, African American obese adults: A post hoc analysis
Steamed broccoli sprouts alleviate DSS-induced inflammation and retain gut microbial biogeography in mice
CNP Research Summary can be found in the CNP Library Membership
Discrimination exposure impacts unhealthy processing of food cues: Crosstalk between the brain and gut
Microbiota from Alzheimer’s patients induce deficits in cognition and hippocampal neurogenesis
Microbial-derived metabolites as a risk factor of age-related cognitive decline and dementia
CNP Research Summary can be found in the CNP Library Membership
Inulin-type fructans and 2’fucosyllactose alter both microbial composition and appear to alleviate stress-induced mood state in a working population compared to placebo (maltodextrin): the EFFICAD Trial, a randomized, controlled trial
Lipids, gut microbiota, and the complex relationship with Alzheimer’s Disease: A narrative review
Neuropsychiatric and neurological diseases in relation to the microbiota-gut-brain axis: From research to clinical care
CNP Research Summary can be found in the CNP Library Membership