Role of gut microbiome in depression
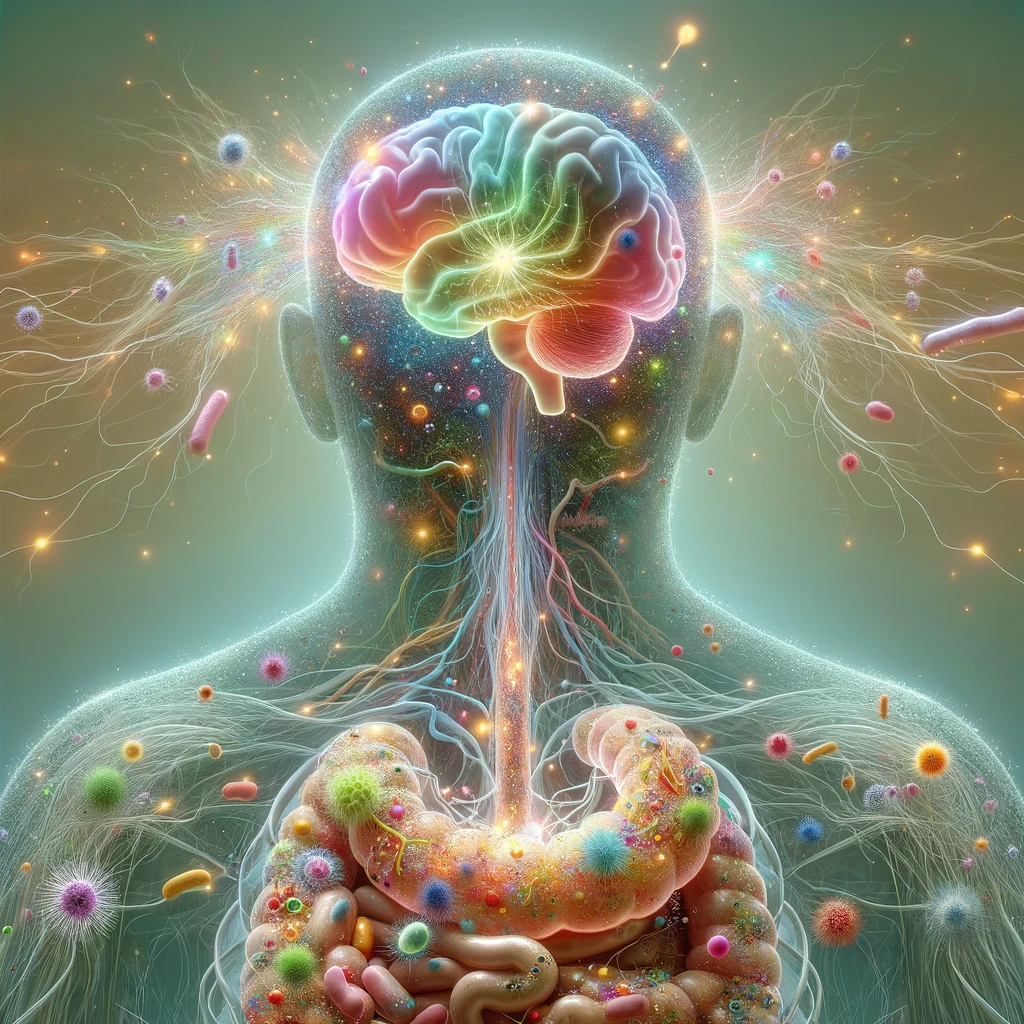
Role of gut microbiome in depression: Beneficial microbes, or probiotics, are increasingly being explored as alternatives to traditional treatments in various fields. This review by Beslin, Humtha & Anju (2025) highlights the positive effects of these microorganisms in enhancing brain function and alleviating depression. It also examines innovative mood enhancement therapies aimed at managing depression. The diversity of gut microbiota has been strongly linked to mood-related behaviors, including major depressive disorder (MDD). This connection is due to the recently identified bidirectional communication system between the gut and brain, which operates through neuroimmune, neuroendocrine, and sensory neural pathways.
Role of gut microbiome in depression
Gut microbes can influence brain function via direct neural signaling through the enteric nervous system (ENS) and vagus nerve, as well as by modulating immune cell activity, affecting behavior and stress responses. The most common kind of dementia, Alzheimer’s disease (AD), is a developing worldwide problem. According to research, the intricate microbial population in the human gut is essential to general health, which includes brain function, owing to the growing evidence on how AD may be impacted by the gut microbiome. A balanced gut microbiota helps maintain brain health by regulating the integrity of biological barriers and metabolic, immune, nervous, and endocrine system functions. However, gut dysbiosis and barrier disruptions can lead to imbalances in these systems, negatively affecting neurological function and promoting AD progression. Potential therapeutic strategies, including fecal microbiota transplants, antibiotics, prebiotics, probiotics, synbiotics, and dietary interventions, are being explored to restore gut microbiome balance and mitigate neurological decline. [NPID: Gut feelings, neurotransmitters, probiotics, serotonin, vagus nerve, Alzheimer’s disease]
Year: 2025
 Navigation
Navigation