Review article: The role of the gut–brain axis in inflammatory bowel disease and its therapeutic implications
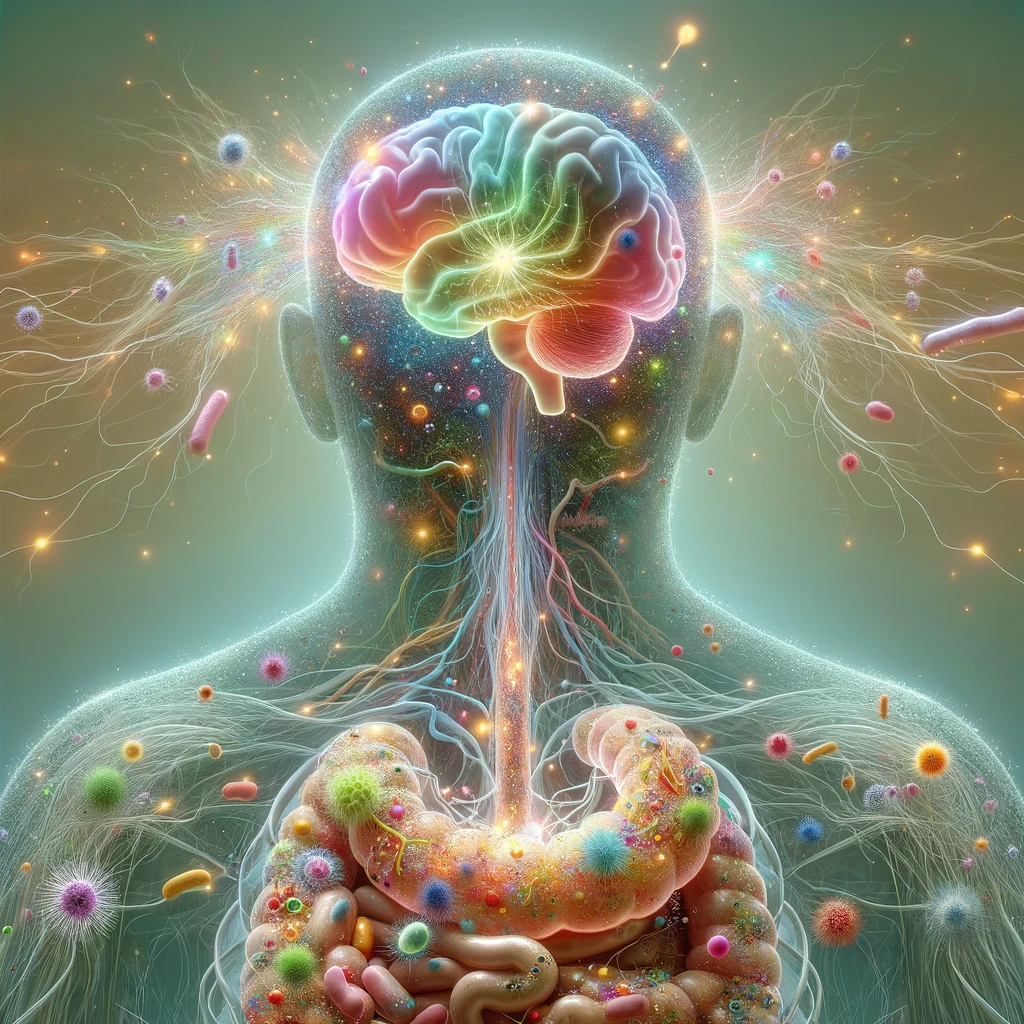
Irritable bowel syndrome (IBS) symptoms have been effectively reduced by treatments that target the gut-brain axis (GBA). People with inflammatory bowel disease (IBD) have much higher rates of common mental illnesses and symptoms similar to IBS, which may indicate that the GBA plays a part in this illness. Manipulating the gut-brain axis could provide new treatment options for certain IBD patients. This review by Riggott, Ford & Gracie (2024) explores the bi-directional relationship between the GBA and IBD and the potential for GBA-focused therapies in managing the condition. The authors searched the Cochrane Central Register of Controlled Trials, EMBASE, MEDLINE, PsychINFO, and EMBASE Classic to locate relevant publications published up until March 2024. The bidirectional interaction between psychological health and the long-term outcomes of disease activity, along with the high rates of IBS-like symptoms, suggests that GBA-mediated effects are at play in IBD. Treatments targeting gut-brain interactions, such as brain-gut behavioral therapies, neuromodulators, and dietary interventions, seem beneficial as adjunct therapies for some patients. Psychological distress is common among IBD patients. The connection between long-term disease outcomes, IBS-like symptom reporting, and poor mental health is mediated through the gut-brain axis. Incorporating proactive psychological management into routine care is recommended. Additional clinical trials of GBA-targeted treatments for patients with co-existing mental health conditions or IBS-like symptoms are needed to develop effective integrated care models in the future. [NPID: Gut-brain axis, inflammatory bowel disease, irritable bowel syndrome, psychological morbidity, GBA-targeted therapies, neuromodulators, brain-gut behavioral treatments]
Year: 2024
 Navigation
Navigation