Implications of the Gut Microbiota for Brain Function and Behavior in Schizophrenia
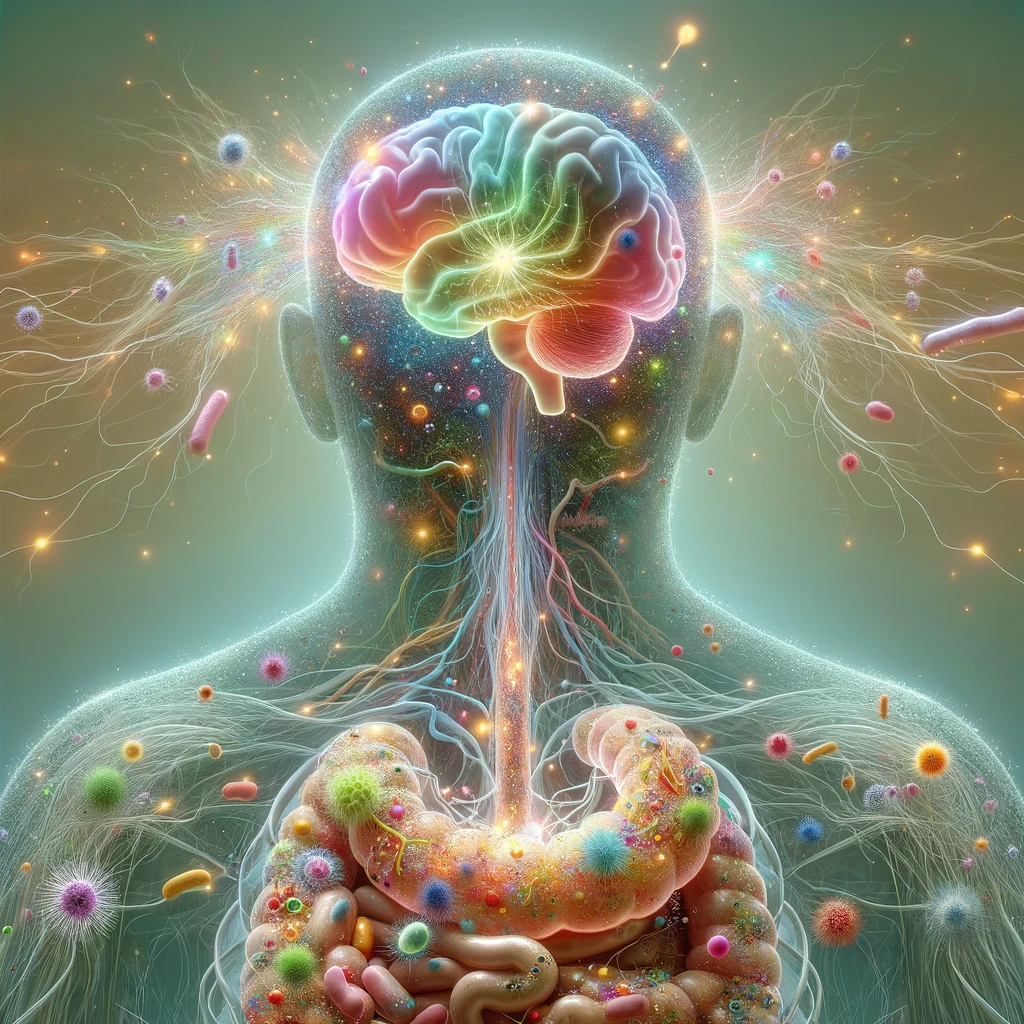
Schizophrenia is a serious, long-term mental illness marked by symptoms such as delusions, hallucinations, cognitive difficulties, and emotional instability, and it often proves challenging to treat. This review by Ansari U. et al. (2024) examines how schizophrenia, a complex psychological disorder, may be related to the gut microbiota—the community of microorganisms living in the digestive tract. The connection between the brain and gut is well-established, and recent studies suggest that an imbalance in the gut microbiome, known as gut dysbiosis, could be linked to schizophrenia. Research comparing the gut microbiota of people with schizophrenia to those without has identified notable differences at both the phylum and genus levels, indicating alterations in the gut microbiome. Enhancing microbiota diversity in schizophrenia patients through dietary changes may help improve their microbiome. Interventions focusing on the gut-brain axis, such as dietary probiotics or prebiotics, could potentially ease some schizophrenia symptoms and enhance patients’ overall well-being. Gaining a deeper understanding of how gut microbiome health interacts with schizophrenia could lead to targeted treatments that modify the gut microbiome, potentially reducing symptoms and improving the quality of life for patients. [NPID: Prebiotics, probiotics, dysbiosis, gut-brain axis, gut microbiota, schizophrenia]
Year: 2024
 Navigation
Navigation





