Gut microbiota in women with eating disorders: A new frontier in pathophysiology and treatment
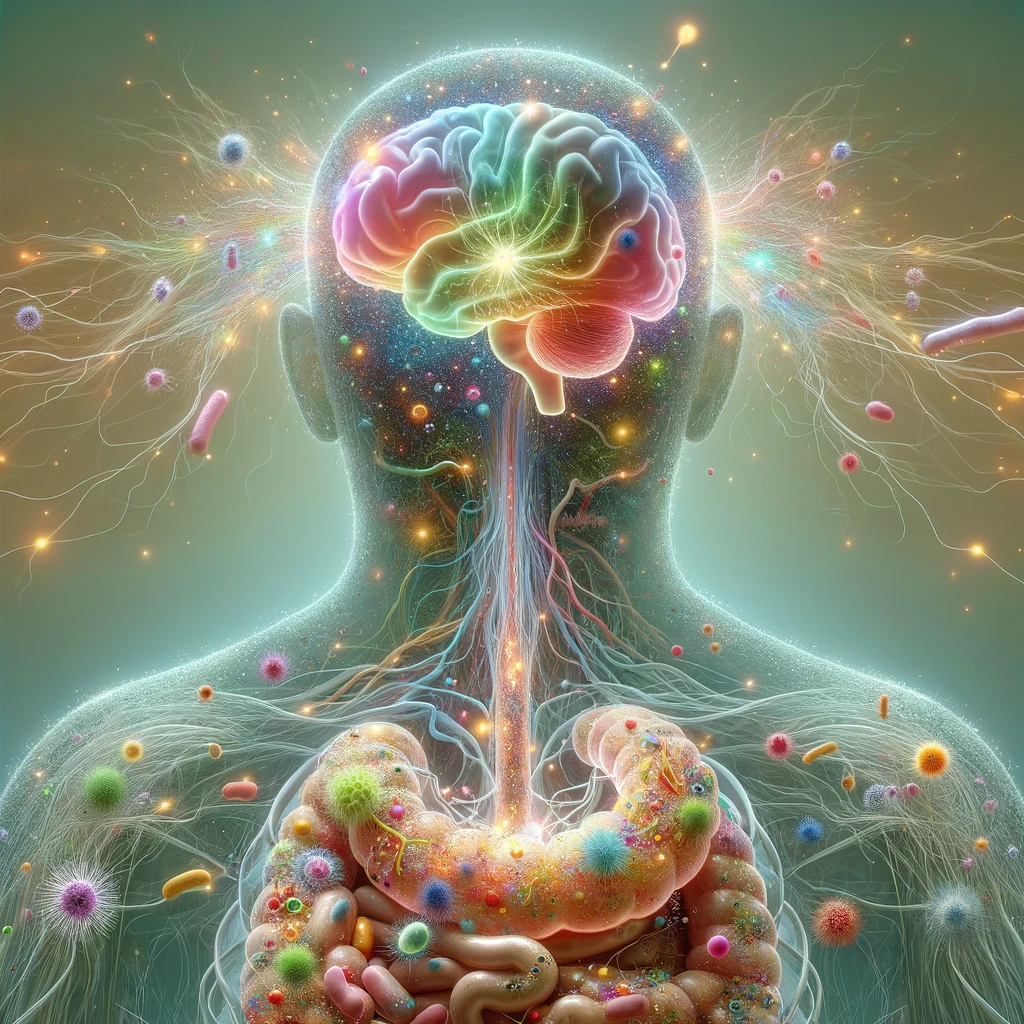
Recent research underscores the important influence of gut microbiota on the development and progression of eating disorders (EDs), especially among women, who are disproportionately affected. The gut microbiota of women suffering from binge eating disorder, bulimia nervosa, and anorexia nervosa is significantly different from that of their healthy counterparts. This imbalance, known as dysbiosis, is characterized by a lower microbial diversity and alterations in key bacteria that are involved in metabolism, inflammation, and communication between the gut and brain. Marano et al. (2025) highlight that the gut microbiome regulates stress, mood, and appetite—all of which are important factors associated with eating disorders. Women’s gut microbiome may be further altered by hormonal changes brought on by menstruation, pregnancy, or menopause, making them more susceptible. Additionally, behaviors common in EDs, such as dietary restriction and purging, worsen these microbial disruptions, leading to increased gut permeability, chronic inflammation, and imbalances in neurotransmitter function. As understanding grows, microbiota-focused treatments—like probiotics, prebiotics, dietary strategies, and fecal microbiota transplants (FMT)—are emerging as potential complements to existing psychological and medical therapies. While approaches such as personalized nutrition and microbiome-based interventions are promising, they are still in their early stages and have not yet been widely proven in clinical settings. Future studies should examine gender-specific microbial patterns, causal relationships, and targeted microbiota treatments to improve care for women with EDs. [NPID: Eating disorders, anorexia nervosa, bulimia nervosa, binge eating disorder, gut microbiota, pathophysiology, microbiota-targeted interventions, women]
Year: 2025
 Navigation
Navigation