Associations between specific dietary patterns, gut microbiome composition, and incident subthreshold depression in Chinese young adults
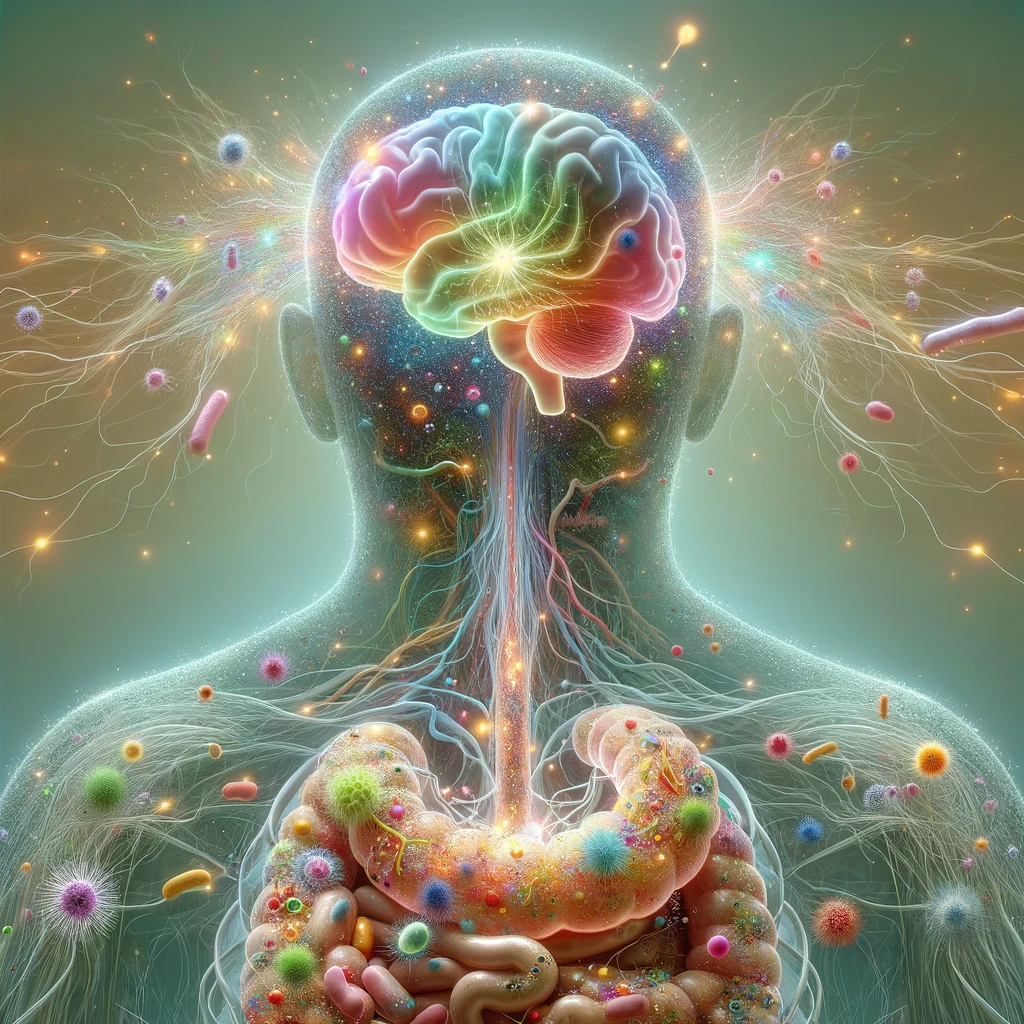
It is unclear how different influencing variables relate to the prevalence of subthreshold depression (SD) among young adults. The purpose of this study by Jiang et al. (2024) was to examine the dietary practices, gut microbiota composition, and other characteristics of young individuals with SD to determine if they are associated with SD. In a cross-sectional design, 178 young persons with SD, ages 18 to 32, were paired with 114 healthy people. To assess SD, the authors used various measurement tools (Beck Depression Inventory-II [BDI-II], Zung Self-Rating Depression Scale [SDS], Hamilton Rating Scales for Depression [HAMD-17], Zung Self-Rating Anxiety Scale [SAS], and the Pittsburgh Sleep Quality Index [PSQI]). Additionally, the authors employed metagenomic sequencing to analyze fecal microbiota profiles and conducted a factor analysis on a 25-item food frequency questionnaire (FFQ) to determine dietary patterns. Dietary habit data was available for 292 participants (mean age 22.1 years; 73.9% female). Logistic regression indicated that dietary patterns I and IV were associated with a lower risk of SD. Participants with SD exhibited distinct microbial profiles, including increased microbial diversity and taxonomic changes. The relationship between a healthy diet that includes foods like potatoes, beans, coarse grains, nuts, fruits, and mushrooms and SD scores (SDS or BDI-II) was discovered to be mediated by Veillonella atypica. The study emphasizes the intricate relationship between young people’s risk of SD, gut flora, and dietary habits. It draws attention to how dietary changes and microbiota modification may be used to support mental wellness. [NPID: Subthreshold depression, dietary patterns, gut microbiota, young adults, microbial diversity, dietary habits, mental health, microbiome modulation]
Year: 2024
 Navigation
Navigation