An association between poor oral health, oral microbiota, and pain identified in New Zealand women with central sensitisation disorders: a prospective clinical study
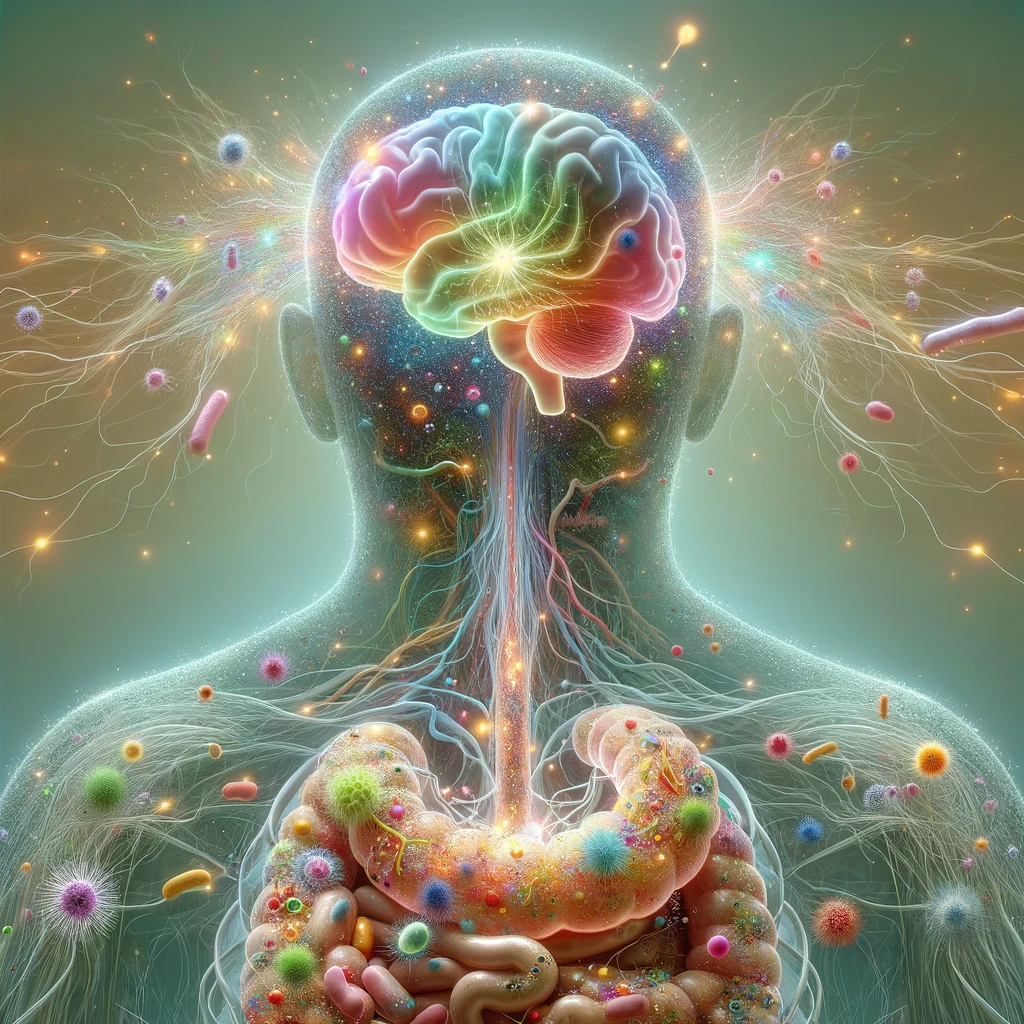
The mouth cavity, the entryway to the gastrointestinal system, contains both transient and permanent microbial communities. Oral pathogens have been linked to the development of several chronic diseases. However, the relationship between oral health, the oral microbiome, and pain in sensitisation disorders has not been thoroughly explored. This study by Erdrich et al. (2025) looked into the relationships between women’s self-reported oral health, oral microbiome, and different kinds of pain. Oral health was evaluated using the WHO oral health questionnaire, while body pain, migraine, and abdominal pain were assessed with validated tools. Saliva samples were analyzed via metatranscriptomics to determine relative gene expression, and demographic and clinical data were examined for links between oral health, pain, and microbiota at three taxonomic levels. Higher degrees of bodily discomfort and migraines were more common in women with worse oral health. Four pathogenic oral species were significantly associated with greater bodily pain, even after adjusting for confounding factors. The genus Gardnerella showed a moderate negative correlation with oral health scores, while Lancefieldella and Mycoplasma salivarius were linked to migraines. Overall, poorer oral health correlated with greater pain and a higher presence of oral pathobionts, suggesting a possible oral microbiome–nervous system connection that may contribute to pain conditions in women. [NPID: Pain, central sensitisation, migraine, functional abdominal pain, oral health, microbiome]
Year: 2025
 Navigation
Navigation